ADVANCING STRATEGIES FOR
Yaws Eradication
Our work in Papua New Guinea has led to the identification of an affordable treatment against yaws that has placed this poverty-related disease on the verge of eradication.
Selected publications
Millat-Martínez, P; Katusele, M; Kasian, B; Omera, E; Jamea, E; Lorry, L (…); Baró, B.
Human and entomological determinants of malaria transmission in the Lihir Islands of Papua New Guinea: A cross-sectional study Journal Article
In: PLOS Neglected Tropical Diseases, vol. 19, iss. 1, 2025.
@article{nokey,
title = {Human and entomological determinants of malaria transmission in the Lihir Islands of Papua New Guinea: A cross-sectional study},
author = {Millat-Martínez, P and Katusele, M and Kasian, B and Omera, E and Jamea, E and Lorry, L (…) and Baró, B. },
doi = {10.1371/journal.pntd.0012277},
year = {2025},
date = {2025-01-03},
urldate = {2025-01-03},
journal = {PLOS Neglected Tropical Diseases},
volume = {19},
issue = {1},
abstract = {Background
The Lihir Islands of Papua New Guinea, located in an area with high burden of malaria and hosting a large mining operation, offer a unique opportunity to study transmission. There, we investigated human and vector factors influencing malaria transmission.
Methods
In 2019, a cross-sectional study was conducted on 2,914 individuals assessing malaria prevalence through rapid diagnostic tests (RDT), microscopy, and quantitative PCR (qPCR). A logistic regression analysis identified infection-associated factors. Anopheles species distribution, biting behaviours, and sporozoite carriage were assessed through human landing catches and larval surveys.
Results
Overall malaria prevalence (any species) was 3.6% by RDT, 4.5% by microscopy, and 15.0% by qPCR. P. vivax accounted for 37.1% of infections, P. falciparum for 34.6%, P. malariae for 3.0%, P. ovale 0.2%, and mixed infections for 24.5%. Prevalence (qPCR) varied across geographic areas, from 8.5% in the mine-impacted zone (MIZ) to 27.0% in the non-MIZ. Other factors independently associated with infection risk included cohabiting with an infected individual (aOR = 1.94, 95%CI: 1.56–2.42), and residing in traditional housing (aOR = 1.65, 95%CI: 1.21–2.25). Children had double the infection risk compared to adults, and the use of long-lasting insecticidal-treated nets did not decrease risk of infection. An. punctulatus was the major vector in one of the four geographical areas; while An. farauti was predominant in the rest of them, both with an early biting behaviour but with different biting intensities by geographical area. Entomological inoculation rates ranged from 26.9 (95%CI: 12.3–45.2) infective bites per person-year in the MIZ to 441.3 (95%CI: 315.7–572.1) in the non-MIZ.
Conclusions
Malaria transmission and infection was lower in the MIZ compared to other areas. Measures focusing on at-risk groups, including vector-control and transmission interruption methods, could be taken into account by the mine and the healthcare authorities to reduce malaria burden outside the MIZ.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
The Lihir Islands of Papua New Guinea, located in an area with high burden of malaria and hosting a large mining operation, offer a unique opportunity to study transmission. There, we investigated human and vector factors influencing malaria transmission.
Methods
In 2019, a cross-sectional study was conducted on 2,914 individuals assessing malaria prevalence through rapid diagnostic tests (RDT), microscopy, and quantitative PCR (qPCR). A logistic regression analysis identified infection-associated factors. Anopheles species distribution, biting behaviours, and sporozoite carriage were assessed through human landing catches and larval surveys.
Results
Overall malaria prevalence (any species) was 3.6% by RDT, 4.5% by microscopy, and 15.0% by qPCR. P. vivax accounted for 37.1% of infections, P. falciparum for 34.6%, P. malariae for 3.0%, P. ovale 0.2%, and mixed infections for 24.5%. Prevalence (qPCR) varied across geographic areas, from 8.5% in the mine-impacted zone (MIZ) to 27.0% in the non-MIZ. Other factors independently associated with infection risk included cohabiting with an infected individual (aOR = 1.94, 95%CI: 1.56–2.42), and residing in traditional housing (aOR = 1.65, 95%CI: 1.21–2.25). Children had double the infection risk compared to adults, and the use of long-lasting insecticidal-treated nets did not decrease risk of infection. An. punctulatus was the major vector in one of the four geographical areas; while An. farauti was predominant in the rest of them, both with an early biting behaviour but with different biting intensities by geographical area. Entomological inoculation rates ranged from 26.9 (95%CI: 12.3–45.2) infective bites per person-year in the MIZ to 441.3 (95%CI: 315.7–572.1) in the non-MIZ.
Conclusions
Malaria transmission and infection was lower in the MIZ compared to other areas. Measures focusing on at-risk groups, including vector-control and transmission interruption methods, could be taken into account by the mine and the healthcare authorities to reduce malaria burden outside the MIZ.
Handley, Becca; González-Beiras, Camila; Tchatchouang, Serges; Hugues, Kouadio Aboh; Basing, Laud Antony; Sylla, Aboubacar (…); Marks, Michael.
A loop-mediated isothermal amplification test for yaws: a multi-country diagnostic accuracy evaluation Journal Article
In: The Lancet Global Health , vol. 12, iss. 11, pp. e1891-e1898, 2024.
@article{nokey,
title = {A loop-mediated isothermal amplification test for yaws: a multi-country diagnostic accuracy evaluation},
author = {Handley, Becca and González-Beiras, Camila and Tchatchouang, Serges and Hugues, Kouadio Aboh and Basing, Laud Antony and Sylla, Aboubacar (…) and Marks, Michael. },
doi = {10.1016/S2214-109X(24)00324-3 },
year = {2024},
date = {2024-11-12},
urldate = {2024-11-12},
journal = {The Lancet Global Health },
volume = {12},
issue = {11},
pages = {e1891-e1898},
abstract = {Background: To meet the WHO target of eradicating yaws by 2030, highly sensitive and specific diagnostic tools are needed. A multiplex Treponema pallidum-Haemophilus ducreyi loop-mediated isothermal amplification (TPHD-LAMP) test holds promise as a near-patient diagnostic tool for yaws and H ducreyi. We conducted a prospective evaluation in Cameroon, Côte d'Ivoire, Ghana, and the Republic of the Congo to determine the diagnostic accuracy of the TPHD-LAMP test, as well as to assess its acceptability, feasibility, and cost.
Methods: Active case searching within schools and communities was used to locate participants with clinically suspicious laws-like lesions. Individuals with serologically confirmed active yaws provided paired lesion swabs between March, 2021, and April, 2023. For each participant, one swab was tested with the TPHD-LAMP at a local district laboratory and the other with reference quantitative PCR (qPCR) tests conducted at national reference laboratories. The primary outcome was TPHD-LAMP test sensitivity and specificity compared with qPCR. Laboratory technicians were interviewed using a multiple-choice survey to gauge acceptability and feasibility of the TPHD-LAMP test. Costs of each test were calculated.
Findings: Of 3085 individuals with at least one suspected yaws lesion, 531 (17%) were serologically confirmed. We enrolled 493 participants with seropositive yaws and a further 32 with negative serology. The sensitivity of the TPHD-LAMP test for detecting T pallidum was 63% (95% CI 56-70) and the specificity was 66% (95% CI 61-71). Sensitivity and specificity for T pallidum improved to 73% (63-82; p=0·0065) and 75% (68-80; p=0·0003), respectively, in H ducreyi-negative samples. Interviews highlighted challenges in user-friendliness and practicality of the TPHD-LAMP test. The cost of the test per sample was one third of that of qPCR, although the TPHD-LAMP test entailed higher costs to establish the assay.
Interpretation: This was the first multi-country diagnostic evaluation of a molecular test for yaws. The TPHD-LAMP testing, in its current form, falls short of the WHO target product profile criteria for yaws diagnostics. These findings highlight the importance of assessing new diagnostics in real-world conditions to ensure their suitability for programmatic use.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Methods: Active case searching within schools and communities was used to locate participants with clinically suspicious laws-like lesions. Individuals with serologically confirmed active yaws provided paired lesion swabs between March, 2021, and April, 2023. For each participant, one swab was tested with the TPHD-LAMP at a local district laboratory and the other with reference quantitative PCR (qPCR) tests conducted at national reference laboratories. The primary outcome was TPHD-LAMP test sensitivity and specificity compared with qPCR. Laboratory technicians were interviewed using a multiple-choice survey to gauge acceptability and feasibility of the TPHD-LAMP test. Costs of each test were calculated.
Findings: Of 3085 individuals with at least one suspected yaws lesion, 531 (17%) were serologically confirmed. We enrolled 493 participants with seropositive yaws and a further 32 with negative serology. The sensitivity of the TPHD-LAMP test for detecting T pallidum was 63% (95% CI 56-70) and the specificity was 66% (95% CI 61-71). Sensitivity and specificity for T pallidum improved to 73% (63-82; p=0·0065) and 75% (68-80; p=0·0003), respectively, in H ducreyi-negative samples. Interviews highlighted challenges in user-friendliness and practicality of the TPHD-LAMP test. The cost of the test per sample was one third of that of qPCR, although the TPHD-LAMP test entailed higher costs to establish the assay.
Interpretation: This was the first multi-country diagnostic evaluation of a molecular test for yaws. The TPHD-LAMP testing, in its current form, falls short of the WHO target product profile criteria for yaws diagnostics. These findings highlight the importance of assessing new diagnostics in real-world conditions to ensure their suitability for programmatic use.
Tchatchouang, Serges; Basing, Laud Antony; Hugues, Kouadio Aboh; Handley, Becca; Gonzalez-Beiras, Camila; Amanor, Ivy (…); Marks, Michael.
An integrated active case detection and management of skin NTDs in yaws endemic health districts in Cameroon, Côte d'Ivoire and Ghana Journal Article
In: PLOS Neglected Tropical Diseases, vol. 18, iss. 10, 2024.
@article{nokey,
title = {An integrated active case detection and management of skin NTDs in yaws endemic health districts in Cameroon, Côte d'Ivoire and Ghana},
author = {Tchatchouang, Serges and Basing, Laud Antony and Hugues, Kouadio Aboh and Handley, Becca and Gonzalez-Beiras, Camila and Amanor, Ivy (…) and Marks, Michael. },
doi = {10.1371/journal.pntd.0011790},
year = {2024},
date = {2024-10-04},
urldate = {2024-10-04},
journal = {PLOS Neglected Tropical Diseases},
volume = {18},
issue = {10},
abstract = {Background: Integrated approaches to mapping skin Neglected Tropical Diseases (NTDs) may be cost-effective way to guide decisions on resource mobilization. Pilot studies have been carried out, but large-scale data covering multiple countries endemic for skin NTDs are lacking. Within the LAMP4YAWS project, we collected integrated data on the burden of multiple skin NTDs.
Methods: From March 2021 to March 2023, integrated case searches for yaws alongside other skin conditions were performed in endemic health districts of yaws in Cameroon, Côte d'Ivoire, and Ghana. Integrated activities included training, social mobilization and active case detection. Initial screening involved a brief clinical examination of participants to determine if any skin conditions were suspected. Cases of skin NTDs were then referred to a health facility for appropriate management.
Results: Overall 61,080 individuals screened, 11,387 (18.6%) had skin lesions. The majority of individuals (>90%) examined were children aged 15 years old and under. The proportion of serologically confirmed yaws cases was 8.6% (18/210) in Cameroon, 6.8% (84/1232) in Côte d'Ivoire, and 26.8% (440/1643) in Ghana. Other skin conditions based on clinical examination included: scabies, Buruli ulcer, leprosy, lymphatic filariasis (lymphoedema and hydrocele), tungiasis, and fungal infections. The most common conditions were scabies and superficial fungal infections. In Cameroon, scabies and superficial fungal infections accounted for 5.1% (214/4204) and 88.7% (3730/4204) respectively, 25.2% (1285/5095) and 50.4% (2567/5095) in Côte d'Ivoire. In Ghana, 20% (419/2090) of individuals had scabies but superficial fungal infections were not routinely recorded and were reported in only 1.3% (28/2090). Other skin NTDs were less common across all three countries.
Conclusion: This study confirms that integrated screening allows simultaneous detection of multiple skin NTDs, maximising use of scarce resources.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Methods: From March 2021 to March 2023, integrated case searches for yaws alongside other skin conditions were performed in endemic health districts of yaws in Cameroon, Côte d'Ivoire, and Ghana. Integrated activities included training, social mobilization and active case detection. Initial screening involved a brief clinical examination of participants to determine if any skin conditions were suspected. Cases of skin NTDs were then referred to a health facility for appropriate management.
Results: Overall 61,080 individuals screened, 11,387 (18.6%) had skin lesions. The majority of individuals (>90%) examined were children aged 15 years old and under. The proportion of serologically confirmed yaws cases was 8.6% (18/210) in Cameroon, 6.8% (84/1232) in Côte d'Ivoire, and 26.8% (440/1643) in Ghana. Other skin conditions based on clinical examination included: scabies, Buruli ulcer, leprosy, lymphatic filariasis (lymphoedema and hydrocele), tungiasis, and fungal infections. The most common conditions were scabies and superficial fungal infections. In Cameroon, scabies and superficial fungal infections accounted for 5.1% (214/4204) and 88.7% (3730/4204) respectively, 25.2% (1285/5095) and 50.4% (2567/5095) in Côte d'Ivoire. In Ghana, 20% (419/2090) of individuals had scabies but superficial fungal infections were not routinely recorded and were reported in only 1.3% (28/2090). Other skin NTDs were less common across all three countries.
Conclusion: This study confirms that integrated screening allows simultaneous detection of multiple skin NTDs, maximising use of scarce resources.
Medappa, Monica; Popisilova, Petra; John, Lucy N.; Gonzalez-Beiras, Camila; Vall-Mayans, Martí; Mitjà, Oriol; Smajs, David
In: PLOS Neglected Tropical Diseases, vol. 18, iss. 8, 2024.
@article{nokey,
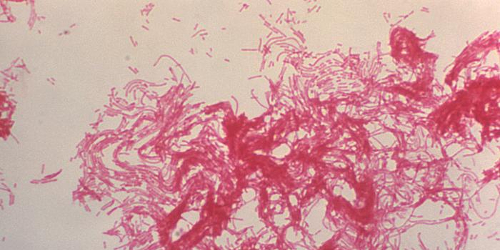
title = {Sequence typing of Haemophilus ducreyi isolated from patients in the Namatanai region of Papua New Guinea: Infections by Class I and Class II strain types differ in ulcer duration and resurgence of infection after azithromycin treatment},
author = {Monica Medappa and Petra Popisilova and Lucy N. John and Camila Gonzalez-Beiras and Martí Vall-Mayans and Oriol Mitjà and David Smajs},
doi = {10.1371/journal.pntd.0012398},
year = {2024},
date = {2024-08-15},
urldate = {2024-08-15},
journal = {PLOS Neglected Tropical Diseases},
volume = {18},
issue = {8},
abstract = {Haemophilus ducreyi (HD) is an important cause of cutaneous ulcers in several endemic regions, including the Western Pacific Region, especially among children. An HD sequence typing on swab samples taken from 1,081 ulcers in the Namatanai district of Papua New Guinea, during the pilot study for treatment of yaws, has been performed using the Grant typing system. Of the 363 samples that tested positive for the 16S rDNA of HD, the dsrA sequences of 270 samples were determined. Altogether they revealed 8 HD strain types circulating in Namatanai, including seven strain types of Class I (I.3, I.4, I.5, I.9, I.10, I.11, I.12) and one strain of Class II (II.3); four Class I types (I.9, I.10, I.11, I.12) were novel. The southern region of Namatanai (Matalai Rural) was identified as the region with the lowest genotype diversity and with most infections caused by HD Class II. The middle and northern subdistricts were affected mainly by HD Class I. Analysis of patient characteristics revealed that Class II HD infections were more often represented by longer-lasting ulcers than Class I HD infections. An increase in the prevalence of the I.10 strain was found after azithromycin administration compared to the untreated population at baseline likely reflecting higher infectivity of HD Class I, and more specifically strain type I.10.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
González-Beiras, Camila; Adingra, Tano; Handley, Becca; Arhinful, Daniel; Tchatchouang, Serges; Houndji, Ahouansou (…); Marks, Michael.
Knowledge, attitudes and practices towards yaws in endemic areas of Ghana, Cameroon and Côte d'Ivoire Journal Article
In: PLOS Neglected Tropical Diseases, vol. 18, iss. 6, 2024.
@article{nokey,
title = { Knowledge, attitudes and practices towards yaws in endemic areas of Ghana, Cameroon and Côte d'Ivoire},
author = {González-Beiras, Camila and Adingra, Tano and Handley, Becca and Arhinful, Daniel and Tchatchouang, Serges and Houndji, Ahouansou (…) and Marks, Michael. },
doi = {10.1371/journal.pntd.0012224},
year = {2024},
date = {2024-06-20},
urldate = {2024-06-20},
journal = {PLOS Neglected Tropical Diseases},
volume = {18},
issue = {6},
abstract = {aws, caused by Treponema pallidum ssp. pertenue, remains a significant public health concern in tropical regions of West Africa and the South Pacific, primarily affecting children in remote areas with limited access to hygiene and sanitation. In this study, conducted in three endemic countries of West Africa where yaws remains a significant public health concern (Ghana, Cameroon, and Côte d'Ivoire), we aimed to assess the knowledge, attitudes, and practices related to yaws among community members, community health workers (CHWs), and traditional healers. The study revealed variations in the perception of causes of yaws among community members: the majority or participants in Ghana attributed yaws to germs (60.2%); in Cameroon the most reported form of transmission was contact with or drinking infected water sources (44.6%); and in Côte d'Ivoire both of these answers were also the most prevalent (60.3% germs and 93.% water sources). A substantial proportion of participants in Côte d'Ivoire also associated yaws with witchcraft and divine punishment (44.8%). Only a small proportion of individuals in Ghana and Côte d'Ivoire correctly identified contact with an infected person as a form of transmission (11.9% and 20.7%, respectively) and less than half in Cameroon (42.6%), although more than 98% of all participants reported avoidance behaviours towards yaws infected people due to fear of getting infected. Most participants expressed a preference for seeking care at hospitals (49.2%, 60.6%, 86.2%) or health care professionals including doctors and nurses (58.5%, 41,5% and 17.2%) if they were diagnosed with yaws, although a quarter of participants in Côte d'Ivoire also sought support from traditional healers. The CHWs interviewed were generally well-trained on yaws causes and treatment options, although they often reported low availability of treatment and diagnostic tests for yaws. Our findings underscore the need for community education, awareness campaigns, ongoing CHW training, and improved access to yaws treatment and diagnostic resources. The data also suggest that collaboration with traditional healers, who usually hold a highly esteemed position in the society, such as giving training on yaws causes and transmission or exchanging knowledge on treatment options, could be beneficial in certain regions, particularly in Côte d'Ivoire.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Medappa, Monica; Popisilova, Petra; Madruga, María Paula; John, Lucy N.; Gonzalez-Beiras, Camila; Grillova, Linda (…); Smajs, David
In: PLOS Neglected Tropical Diseases, vol. 18, iss. 1, 2024.
@article{nokey,
title = {Low genetic diversity of Treponema pallidum ssp. pertenue (TPE) isolated from patients' ulcers in Namatanai District of Papua New Guinea: Local human population is infected by three TPE genotypes},
author = {Monica Medappa and Petra Popisilova and María Paula Madruga and Lucy N. John and Camila Gonzalez-Beiras and Grillova, Linda (…) and Smajs, David},
doi = {10.1371/journal.pntd.0011831},
year = {2024},
date = {2024-01-02},
urldate = {2024-01-02},
journal = {PLOS Neglected Tropical Diseases},
volume = {18},
issue = {1},
abstract = {Yaws is an endemic disease caused by Treponema pallidum subsp. pertenue (TPE) that primarily affects children in rural regions of the tropics. The endemic character of yaws infections and the expected exclusive reservoir of TPE in humans opened a new opportunity to start a yaws eradication campaign. We have developed a multi-locus sequence typing (MLST) scheme for TPE isolates combining the previously published (TP0548, TP0488) and new (TP0858) chromosomal loci, and we compared this typing scheme to the two previously published MLST schemes. We applied this scheme to TPE-containing clinical isolates obtained during a mass drug administration study performed in the Namatanai District of Papua New Guinea between June 2018 and December 2019. Of 1081 samples collected, 302 (28.5%) tested positive for TPE DNA, from which 255 (84.4%) were fully typed. The TPE PCR-positivity in swab samples was higher in younger patients, patients with single ulcers, first ulcer episodes, and with ulcer duration less than six months. Non-treponemal serological test positivity correlated better with PCR positivity compared to treponema-specific serological tests. The MLST revealed a low level of genetic diversity among infecting TPE isolates, represented by just three distinct genotypes (JE11, SE22, and TE13). Two previously used typing schemes revealed similar typing resolutions. Two new alleles (one in TP0858 and one in TP0136) were shown to arise by intragenomic recombination/deletion events. Compared to samples genotyped as JE11, the minor genotypes (TE13 and SE22) were more frequently detected in samples from patients with two or more ulcers and patients with higher values of specific TP serological tests. Moreover, the A2058G mutation in the 23S rRNA genes of three JE11 isolates was found, resulting in azithromycin resistance.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Ndzomo, Philippe; Tchatchouang, Serges; Tabah, Ernest; Njamsshi, Theophilus; Noah Tsanga, Mireille Victorine; Bondi, Jules Alexis (…); Eyangoh, Sara
Prevalence and risk factors associated with Haemophilus ducreyi cutaneous ulcers in Cameroon Journal Article
In: PLOS Neglected Tropical Diseases, vol. 17, iss. 12, 2023.
@article{nokey,
title = {Prevalence and risk factors associated with Haemophilus ducreyi cutaneous ulcers in Cameroon},
author = {Ndzomo, Philippe and Tchatchouang, Serges and Tabah, Ernest and Njamsshi, Theophilus and Noah Tsanga, Mireille Victorine and Bondi, Jules Alexis (…) and Eyangoh, Sara},
doi = {10.1371/journal.pntd.0011553},
year = {2023},
date = {2023-12-27},
journal = {PLOS Neglected Tropical Diseases},
volume = {17},
issue = {12},
abstract = {Epidemics of yaws-like cutaneous ulcers are regularly documented in children in the tropics. They occur mainly in poor and remote communities without access to health facilities. The integration of molecular tools into yaws control efforts has made it possible to describe Haemophilus ducreyi (HD) as a major cause of cutaneous ulcers. The objective of this study was to determine the prevalence of HD as cause of cutaneous ulcers, investigate its presence in asymptomatic individuals and identify associated risk factors. A cross-sectional study was conducted in yaws endemic districts of Cameroon. Participants included people presenting yaws-like ulcers and asymptomatic individuals. Swab samples were collected from each participant and tested for HD and Treponema pallidum (TP) using an established qPCR method. Additionally, demographic, habitat, proximity, and hygiene characteristics were collected using a structured questionnaire. A total of 443 individuals participated in the study, including 271 ulcer cases and 172 asymptomatic contacts. The prevalence of HD in ulcers was 30.3% (Confidence Interval (CI) 95% [24.8-35.7]) and the prevalence of asymptomatic HD carriage was 8.6% (CI95% [4.5-12.9]). TP was also detected in our sample among ulcer cases but in lower proportion (5.2% CI95% [2.5-7.8]) compared to HD. The adjusted logistic regression model showed that women were as much at risk of having HD cutaneous ulcer as men regardless of age. Physical proximity to a confirmed ulcer case was the major factor identified favouring HD transmission. HD ulcers were more likely to be present on Bantu individuals compared to Baka as well as HD colonization. These findings highlight HD as the most common cause of cutaneous ulcers in yaws-endemic communities in Cameroon. The exact implications of detecting HD on intact skin are not yet clear. Further studies are needed to understand the significance of this carriage in the spread dynamics of the disease.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Suñer, Clara; John, Lucy N; Houinei, Wendy; Ubals, Maria; Ouchi, Dan; Alemany, Andrea (…); González-Beiras, Camila
Rapid Serologic Test for Diagnosis of Yaws in Patients with Suspicious Skin Ulcers Journal Article
In: Emerging Infectious Diseases, vol. 29, iss. 8, 2023.
@article{nokey,
title = {Rapid Serologic Test for Diagnosis of Yaws in Patients with Suspicious Skin Ulcers},
author = {Clara Suñer and Lucy N John and Wendy Houinei and Maria Ubals and Dan Ouchi and Alemany, Andrea (…) and González-Beiras, Camila},
doi = {10.3201/eid2908.230608},
year = {2023},
date = {2023-08-29},
urldate = {2023-08-29},
journal = {Emerging Infectious Diseases},
volume = {29},
issue = {8},
abstract = {The Chembio DPP (Dual Path Platform) Syphilis Screen & Confirm kit (https://chembio.com) is a rapid serologic test that can be used to diagnose yaws. We evaluated its capacity to detect patients with ulcers that tested PCR positive for Treponema pallidum subsp. pertenue. DPP detected 84% of ulcers that were positive by PCR.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Alshehri, Abdullah; Chhonker, Yashpal S.; Bala, Veenu; Edi, Constant; Bjerum, Catherine M.; Koudou, Benjamin G (…); Murry, Daryl.
Population pharmacokinetic model of ivermectin in mass drug administration against lymphatic filariasis Journal Article
In: PLOS Neglected Tropical Diseases, vol. 17, no. 6, pp. 1-17, 2023.
@article{10.1371/journal.pntd.0011319b,
title = {Population pharmacokinetic model of ivermectin in mass drug administration against lymphatic filariasis},
author = {Abdullah Alshehri and Yashpal S. Chhonker and Veenu Bala and Constant Edi and Catherine M. Bjerum and Koudou, Benjamin G (…) and Murry, Daryl.},
doi = {10.1371/journal.pntd.0011319},
year = {2023},
date = {2023-01-01},
urldate = {2023-01-01},
journal = {PLOS Neglected Tropical Diseases},
volume = {17},
number = {6},
pages = {1-17},
publisher = {Public Library of Science},
abstract = {Background Ivermectin (IVM) is a broad–spectrum anthelmintic drug used to treat diseases caused by filarial worms, such as onchocerciasis and lymphatic filariasis (LF). IVM is part of a triple–drug therapy used by the Mass Drug Administration (MDA) as a preventive strategy to eradicate LF in sub–Saharan Africa. The drug shows high variability in drug exposure in previous pharmacokinetic studies. This study aims to build a population pharmacokinetic (PopPK) model to identify and quantify the possible sources of the variability of IVM exposure after a single–oral dose in LF–infected subjects and healthy individuals. Methodology / Principal findings In this analysis, 724 samples were collected from treatment–naïve Wuchereria bancrofti–infected (n = 32) and uninfected (n = 24) adults living in Côte d’Ivoire who had received one dose of IVM as a part of triple–drug therapy. PopPK analysis was conducted using Phoenix NLME 8.3 software. The Monte Carlo simulation based on the final model was performed to simulate drug exposure among different dosing groups (200 μg/kg, 18 mg, and 36 mg). A two–compartment model with zero–order dose input into the absorption compartment with a lag time function followed by first–order absorption and linear elimination best described the IVM’s pharmacokinetic (PK) parameters. The final model identifies that the PK parameters of IVM are not affected by LF infection. Sex was a significant covariate on the peripheral volume of distribution (Vp/F, 53% lower in men than in women). IVM drug exposure shows linear pharmacokinetic behavior among the simulated dosing groups with similar drug exposure based on sex. Conclusion/Significance We have developed a PopPk model to describe and identify possible sources of the variability of IVM exposure. To our knowledge, this is the first PopPK study of IVM in patients with LF. Trial registration NCT02845713; NCT03664063},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
John, Lucy N.; Beiras, Camila G.; Houinei, Wendy; Medappa, Monica; Sabok, Maria; Kolmau, Reman (…); Mitjà, Oriol.
Trial of Three Rounds of Mass Azithromycin Administration for Yaws Eradication Journal Article
In: New England Journal of Medicine, vol. 386, no. 1, pp. 47-56, 2022.
@article{Lucy2022b,
title = {Trial of Three Rounds of Mass Azithromycin Administration for Yaws Eradication},
author = {Lucy N. John and Camila G. Beiras and Wendy Houinei and Monica Medappa and Maria Sabok and Kolmau, Reman (…) and Mitjà, Oriol.},
doi = {https://doi.org/10.1056/NEJMoa2109449},
year = {2022},
date = {2022-01-01},
urldate = {2022-01-01},
journal = {New England Journal of Medicine},
volume = {386},
number = {1},
pages = {47-56},
abstract = {textitTreponema pallidum subspecies textitpertenue causes yaws. Strategies to better control, eliminate, and eradicate yaws are needed. In an open-label, cluster-randomized, community-based trial conducted in a yaws-endemic area of Papua New Guinea, we randomly assigned 38 wards (i.e., clusters) to receive one round of mass administration of azithromycin followed by two rounds of target treatment of active cases (control group) or three rounds of mass administration of azithromycin (experimental group); round 1 was administered at baseline, round 2 at 6 months, and round 3 at 12 months. The coprimary end points were the prevalence of active cases of yaws, confirmed by polymerase-chain-reaction assay, in the entire trial population and the prevalence of latent yaws, confirmed by serologic testing, in a subgroup of asymptomatic children 1 to 15 years of age; prevalences were measured at 18 months, and the between-group differences were calculated.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
John, Lucy N.; Gonzalez-Beiras, Camila; Vall-Mayans, Marti; Kolmau, Reman; Houinei, Wendy; Wangi, James; Marks, Michael; Mitjà, Oriol
In: The Lancet Regional Health – Western Pacific, 2021, ISSN: 2666-6065.
@article{Lucy2021,
title = {Safety of mass drug coadministration with ivermectin, diethylcarbamazine, albendazole, and azithromycin for the integrated treatment of neglected tropical diseases: a cluster randomized community trial},
author = {Lucy N. John and Camila Gonzalez-Beiras and Marti Vall-Mayans and Reman Kolmau and Wendy Houinei and James Wangi and Michael Marks and Mitjà, Oriol},
doi = {https://doi.org/10.1016/j.lanwpc.2021.100293},
issn = {2666-6065},
year = {2021},
date = {2021-01-01},
urldate = {2021-01-01},
journal = {The Lancet Regional Health – Western Pacific},
publisher = {Elsevier},
abstract = {Neglected tropical diseases control programmes run separately. For settings with more than one endemic disease, combined mass drug administration (MDA) has potential practical advantages compared with separate programmes but needs confirmation of safety. We assessed the safety of combined MDA for multiple neglected tropical diseases using ivermectin, diethylcarbamazine, albendazole (IDA) and azithromycin (AZI).},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Grant, Jacob C; González-Beiras, Camila; Amick, Kristen M; Fortney, Kate R; Gangaiah, Dharanesh; Humphreys, Tricia L (…); Spinola, Stanley M.
Multiple Class I and Class II Haemophilus ducreyi Strains Cause Cutaneous Ulcers in Children on an Endemic Island Journal Article
In: Clinical Infectious Diseases, vol. 11, iss. 67, pp. 1768-1774, 2018.
@article{10.1093/cid/ciy343,
title = {Multiple Class I and Class II Haemophilus ducreyi Strains Cause Cutaneous Ulcers in Children on an Endemic Island},
author = {Jacob C Grant and Camila González-Beiras and Kristen M Amick and Kate R Fortney and Dharanesh Gangaiah and Humphreys, Tricia L (…) and Spinola, Stanley M.},
doi = {10.1093/cid/ciy343},
year = {2018},
date = {2018-11-13},
urldate = {2018-11-13},
journal = {Clinical Infectious Diseases},
volume = {11},
issue = {67},
pages = {1768-1774},
abstract = {Background: Together with Treponema pallidum subspecies pertenue, Haemophilus ducreyi is a major cause of exudative cutaneous ulcers (CUs) in children. For H. ducreyi, both class I and class II strains, asymptomatic colonization, and environmental reservoirs have been found in endemic regions, but the epidemiology of this infection is unknown.
Methods: Based on published whole-genome sequences of H. ducreyi CU strains, a single-locus typing system was developed and applied to H. ducreyi-positive CU samples obtained prior to, 1 year after, and 2 years after the initiation of a mass drug administration campaign to eradicate CU on Lihir Island in Papua New Guinea. DNA from the CU samples was amplified with class I and class II dsrA-specific primers and sequenced; the samples were classified into dsrA types, which were geospatially mapped. Selection pressure analysis was performed on the dsrA sequences.
Results: Thirty-seven samples contained class I sequences, 27 contained class II sequences, and 13 contained both. There were 5 class I and 4 class II types circulating on the island; 3 types accounted for approximately 87% of the strains. The composition and geospatial distribution of the types varied little over time and there was no evidence of selection pressure.
Conclusions: Multiple strains of H. ducreyi cause CU on an endemic island and coinfections are common. In contrast to recent findings with T. pallidum pertenue, strain composition is not affected by antibiotic pressure, consistent with environmental reservoirs of H. ducreyi. Such reservoirs must be addressed to achieve eradication of H. ducreyi.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Methods: Based on published whole-genome sequences of H. ducreyi CU strains, a single-locus typing system was developed and applied to H. ducreyi-positive CU samples obtained prior to, 1 year after, and 2 years after the initiation of a mass drug administration campaign to eradicate CU on Lihir Island in Papua New Guinea. DNA from the CU samples was amplified with class I and class II dsrA-specific primers and sequenced; the samples were classified into dsrA types, which were geospatially mapped. Selection pressure analysis was performed on the dsrA sequences.
Results: Thirty-seven samples contained class I sequences, 27 contained class II sequences, and 13 contained both. There were 5 class I and 4 class II types circulating on the island; 3 types accounted for approximately 87% of the strains. The composition and geospatial distribution of the types varied little over time and there was no evidence of selection pressure.
Conclusions: Multiple strains of H. ducreyi cause CU on an endemic island and coinfections are common. In contrast to recent findings with T. pallidum pertenue, strain composition is not affected by antibiotic pressure, consistent with environmental reservoirs of H. ducreyi. Such reservoirs must be addressed to achieve eradication of H. ducreyi.
Mitjà, Oriol; Godornes, Charmie; Houinei, Wendy; Kapa, August; Paru, Raymond; Abel, Haina (…); Lukehart, Sheila A.
Re-emergence of yaws after single mass azithromycin treatment followed by targeted treatment: a longitudinal study Journal Article
In: The Lancet, vol. 391, no. 10130, pp. 1599-1607, 2018, ISSN: 0140-6736.
@article{Mitjà2018,
title = {Re-emergence of yaws after single mass azithromycin treatment followed by targeted treatment: a longitudinal study},
author = {Oriol Mitjà and Charmie Godornes and Wendy Houinei and August Kapa and Raymond Paru and Abel, Haina (…) and Lukehart, Sheila A.},
doi = {10.1016/S0140-6736(18)30204-6},
issn = {0140-6736},
year = {2018},
date = {2018-01-01},
urldate = {2018-01-01},
journal = {The Lancet},
volume = {391},
number = {10130},
pages = {1599-1607},
publisher = {Elsevier},
abstract = {Yaws is a substantial cause of chronic disfiguring ulcers in children in at least 14 countries in the tropics. WHO's newly adopted strategy for yaws eradication uses a single round of mass azithromycin treatment followed by targeted treatment programmes, and data from pilot studies have shown a short-term significant reduction of yaws. We assessed the long-term efficacy of the WHO strategy for yaws eradication.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Marks, Michael; Mitjà, Oriol; Bottomley, Christian; Kwakye, Cynthia; Houinei, Wendy; Bauri, Mathias (…); Wanaom, Augustine.
In: The Lancet Global Health, vol. 6, no. 4, pp. e401-e410, 2018, ISSN: 2214-109X.
@article{Marks2018,
title = {Comparative efficacy of low-dose versus standard-dose azithromycin for patients with yaws: a randomised non-inferiority trial in Ghana and Papua New Guinea},
author = {Michael Marks and Oriol Mitjà and Christian Bottomley and Cynthia Kwakye and Wendy Houinei and Bauri, Mathias (…) and Wanaom, Augustine.},
doi = {10.1016/S2214-109X(18)30023-8},
issn = {2214-109X},
year = {2018},
date = {2018-01-01},
urldate = {2018-01-01},
journal = {The Lancet Global Health},
volume = {6},
number = {4},
pages = {e401-e410},
publisher = {Elsevier},
abstract = {A dose of 30 mg/kg of azithromycin is recommended for treatment of yaws, a disease targeted for global eradication. Treatment with 20 mg/kg of azithromycin is recommended for the elimination of trachoma as a public health problem. In some settings, these diseases are co-endemic. We aimed to determine the efficacy of 20 mg/kg of azithromycin compared with 30 mg/kg azithromycin for the treatment of active and latent yaws.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
González-Beiras, Camila; Kapa, August; Vall-Mayans, Marti; Paru, Raymond; Gavilán, Sergi; Houinei, Wendy (…); Mitjà, Oriol.
Single-Dose Azithromycin for the Treatment of Haemophilus ducreyi Skin Ulcers in Papua New Guinea Journal Article
In: Clinical Infectious Diseases, vol. 65, iss. 12, pp. 2085–2090, 2017.
@article{10.1093/cid/cix723,
title = {Single-Dose Azithromycin for the Treatment of Haemophilus ducreyi Skin Ulcers in Papua New Guinea},
author = {Camila González-Beiras and August Kapa and Marti Vall-Mayans and Raymond Paru and Sergi Gavilán and Houinei, Wendy (…) and Mitjà, Oriol. },
doi = {10.1093/cid/cix723},
year = {2017},
date = {2017-08-16},
urldate = {2017-08-16},
journal = {Clinical Infectious Diseases},
volume = {65},
issue = {12},
pages = {2085–2090},
abstract = {Background
Haemophilus ducreyi (HD) and Treponema pallidum subspecies pertenue (TP) are major causative agents of cutaneous ulcer (CU) in the tropics. Azithromycin is recommended to treat sexually transmitted HD infections and has good in vitro activity against HD strains from both genital and skin ulcers. We investigated the efficacy of oral single-dose azithromycin on HD-CU.
Methods
We conducted a community-based cohort study in Lihir Island, Papua New Guinea, from October 2014 through May 2016. Consenting patients with skin ulcers >1 cm in diameter were eligible for this study and had collected a lesional swab for polymerase chain reaction (PCR). All participants were treated with single-dose azithromycin (30 mg/kg) and were followed up for assessment of clinical resolution. We retrospectively classified patients according to PCR results into HD, TP, and PCR-negative groups. The primary endpoint was healing rates of HD-CU at 14 days after treatment.
Results
We obtained full outcome data from 246 patients; 131 (53.3%) were HD PCR positive, 37 (15.0%) were TP positive, and 78 (31.7%) were negative for all tests. Healing rates were 88.5% (95% confidence interval [CI], .82–.93) in the HD group, 78.4% [95% CI, .63–.89] in the TP group, and 74.4% (95% CI, .64–.83) in the PCR-negative group. If we included the participants with improved ulcers, the healing rates increased to 94.7%, 97.3%, and 89.7% respectively. HD cases classified as not healed all converted to HD-negative PCR.
Conclusions
Based upon clinical resolution and PCR conversion to HD negative, a single oral dose of azithromycin is efficacious for the treatment of HD-CU. These results have implications for the treatment of individual patients and for the use of antibiotics in public health strategies to control CU in the tropics.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Haemophilus ducreyi (HD) and Treponema pallidum subspecies pertenue (TP) are major causative agents of cutaneous ulcer (CU) in the tropics. Azithromycin is recommended to treat sexually transmitted HD infections and has good in vitro activity against HD strains from both genital and skin ulcers. We investigated the efficacy of oral single-dose azithromycin on HD-CU.
Methods
We conducted a community-based cohort study in Lihir Island, Papua New Guinea, from October 2014 through May 2016. Consenting patients with skin ulcers >1 cm in diameter were eligible for this study and had collected a lesional swab for polymerase chain reaction (PCR). All participants were treated with single-dose azithromycin (30 mg/kg) and were followed up for assessment of clinical resolution. We retrospectively classified patients according to PCR results into HD, TP, and PCR-negative groups. The primary endpoint was healing rates of HD-CU at 14 days after treatment.
Results
We obtained full outcome data from 246 patients; 131 (53.3%) were HD PCR positive, 37 (15.0%) were TP positive, and 78 (31.7%) were negative for all tests. Healing rates were 88.5% (95% confidence interval [CI], .82–.93) in the HD group, 78.4% [95% CI, .63–.89] in the TP group, and 74.4% (95% CI, .64–.83) in the PCR-negative group. If we included the participants with improved ulcers, the healing rates increased to 94.7%, 97.3%, and 89.7% respectively. HD cases classified as not healed all converted to HD-negative PCR.
Conclusions
Based upon clinical resolution and PCR conversion to HD negative, a single oral dose of azithromycin is efficacious for the treatment of HD-CU. These results have implications for the treatment of individual patients and for the use of antibiotics in public health strategies to control CU in the tropics.
Mitjà, Oriol; González-Beiras, Camila; Godornes, Charmie; Kolmau, Reman; Houinei, Wendy; Abel, Haina (…); Bassat, Quique.
Effectiveness of single-dose azithromycin to treat latent yaws: a longitudinal comparative cohort study Journal Article
In: The Lancet Global Health, vol. 5, no. 12, pp. e1268-e1274, 2017, ISSN: 2214-109X.
@article{Mitjà2017,
title = {Effectiveness of single-dose azithromycin to treat latent yaws: a longitudinal comparative cohort study},
author = {Oriol Mitjà and Camila González-Beiras and Charmie Godornes and Reman Kolmau and Wendy Houinei and Abel, Haina (…) and Bassat, Quique.},
doi = {10.1016/S2214-109X(17)30388-1},
issn = {2214-109X},
year = {2017},
date = {2017-01-01},
urldate = {2017-01-01},
journal = {The Lancet Global Health},
volume = {5},
number = {12},
pages = {e1268-e1274},
publisher = {Elsevier},
abstract = {Treatment of latent yaws is a crucial component of the WHO yaws eradication strategy to prevent relapse and the resulting transmission to uninfected children. We assessed the effectiveness of single-dose azithromycin to treat patients with latent yaws.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Houinei, Wendy; Godornes, Charmie; Kapa, August; Knauf, Sascha; Mooring, Eric Q.; González-Beiras, Camila (…); Mitjà, Oriol.
Haemophilus ducreyi DNA is detectable on the skin of asymptomatic children, flies and fomites in villages of Papua New Guinea Journal Article
In: PLOS Neglected Tropical Diseases, vol. 11, no. 5, pp. 1-10, 2017.
@article{10.1371/journal.pntd.0004958,
title = {Haemophilus ducreyi DNA is detectable on the skin of asymptomatic children, flies and fomites in villages of Papua New Guinea},
author = {Wendy Houinei and Charmie Godornes and August Kapa and Sascha Knauf and Eric Q. Mooring and González-Beiras, Camila (…) and Mitjà, Oriol. },
doi = {10.1371/journal.pntd.0004958},
year = {2017},
date = {2017-01-01},
urldate = {2017-01-01},
journal = {PLOS Neglected Tropical Diseases},
volume = {11},
number = {5},
pages = {1-10},
publisher = {Public Library of Science},
abstract = {Author summary Children in rural communities of tropical countries often suffer skin ulcers that are caused by the bacteria Haemophilus ducreyi–causative agent of chancroid- and Treponema pallidum subsp. pertenue -causative agent of yaws-. The currently recommended strategy for yaws eradication is one round of mass drug administration (MDA) with azithromycin. We attempted to find reasons for the limited impact of yaws MDA on the prevalence of H. ducreyi leg ulcers by examining potential sources of infection in healthy carriers, flies, and bed linen. H. ducreyi DNA was found in skin swabs from 20% of asymptomatic children, in 9/10 flies, and 3/6 bed sheets from the houses of children with ulcers. While H. ducreyi DNA has been detected in the genital tract of asymptomatic women without genital ulcers, this is the first report of such detection on the skin of asymptomatic individuals. Importantly, skin cultures obtained from two asymptomatic children yielded viable H. ducreyi, confirming colonization and a potential reservoir of infection. If confirmed to contain viable bacteria, flies and fomites may also contribute to the continued presence of this infection after mass treatment with azithromycin. Our findings provide evidence that persistence of H. ducreyi ulcers after antibiotic MDA is due to the ubiquity of the organism in the environment. Improved hygiene and additional strategies such as repeated rounds of MDA could be able to control such a reservoir.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
González-Beiras, Camila; Marks, Michael; Chen, Cheng; Roberts, Sally; Mitjà, Oriol
Epidemiology of Haemophilus ducreyi Infections Journal Article
In: Emerging Infectious Diseases, vol. 22, no. 1, pp. 1-8, 2016.
@article{Gonzalez2016,
title = {Epidemiology of Haemophilus ducreyi Infections},
author = {Camila González-Beiras and Michael Marks and Cheng Chen and Sally Roberts and Oriol Mitjà},
doi = {10.3201/eid2201.150425},
year = {2016},
date = {2016-01-01},
urldate = {2016-01-01},
journal = {Emerging Infectious Diseases},
volume = {22},
number = {1},
pages = {1-8},
publisher = {CDC},
abstract = {The global epidemiology of emphHaemophilus ducreyi infections is poorly documented because of difficulties in confirming microbiological diagnoses. We evaluated published data on the proportion of genital and nongenital skin ulcers caused by emphH. ducreyi before and after introduction of syndromic management for genital ulcer disease (GUD). Before 2000, the proportion of GUD caused by emphH. ducreyi ranged from 0.0% to 69.0% (35 studies in 25 countries). After 2000, the proportion ranged from 0.0% to 15.0% (14 studies in 13 countries). In contrast, emphH. ducreyi has been recently identified as a causative agent of skin ulcers in children in the tropical regions; proportions ranged from 9.0% to 60.0% (6 studies in 4 countries). We conclude that, although there has been a sustained reduction in the proportion of GUD caused by emphH. ducreyi, this bacterium is increasingly recognized as a major cause of nongenital cutaneous ulcers.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mitjà, Oriol; Houinei, Wendy; Moses, Penias; Kapa, August; Paru, Raymond; Hays, Russell (…); Bassat, Quique.
Mass Treatment with Single-Dose Azithromycin for Yaws Journal Article
In: New England Journal of Medicine, vol. 372, no. 8, pp. 703-710, 2015.
@article{Oriol2015,
title = {Mass Treatment with Single-Dose Azithromycin for Yaws},
author = {Oriol Mitjà and Wendy Houinei and Penias Moses and August Kapa and Raymond Paru and Hays, Russell (…) and Bassat, Quique. },
doi = {10.1056/NEJMoa1408586},
year = {2015},
date = {2015-01-01},
urldate = {2015-01-01},
journal = {New England Journal of Medicine},
volume = {372},
number = {8},
pages = {703-710},
abstract = {Mass treatment with azithromycin is a central component of the new World Health Organization (WHO) strategy to eradicate yaws. Empirical data on the effectiveness of the strategy are required as a prerequisite for worldwide implementation of the plan.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Marks, Michael; Mitjà, Oriol; Vestergaard, Lasse S.; Pillay, Allan; Knauf, Sascha; Chen, Cheng-Yen (…); Asiedu, Kingsley B.
Challenges and key research questions for yaws eradication Journal Article
In: The Lancet Infectious Diseases, vol. 15, no. 10, pp. 1220-1225, 2015, ISSN: 1473-3099.
@article{Marks2015,
title = {Challenges and key research questions for yaws eradication},
author = {Michael Marks and Oriol Mitjà and Lasse S. Vestergaard and Allan Pillay and Sascha Knauf and Chen, Cheng-Yen (…) and Asiedu, Kingsley B.},
doi = {10.1016/S1473-3099(15)00136-X},
issn = {1473-3099},
year = {2015},
date = {2015-01-01},
urldate = {2015-01-01},
journal = {The Lancet Infectious Diseases},
volume = {15},
number = {10},
pages = {1220-1225},
publisher = {Elsevier},
abstract = {Yaws is endemic in west Africa, southeast Asia, and the Pacific region. To eradicate yaws by 2020, WHO has launched a campaign of mass treatment with azithromycin. Progress has been made towards achievement of this ambitious goal, including the validation of point-of-care and molecular diagnostic tests and piloting of the strategy in several countries, including Ghana, Vanuatu, and Papua New Guinea. Gaps in knowledge need to be addressed to allow refinement of the eradication strategy. Studies exploring determinants of the spatial distribution of yaws are needed to help with the completion of baseline mapping. The finding that emphHaemophilus ducreyi causes lesions similar to yaws is particularly important and further work is needed to assess the effect of azithromycin on these lesions. The integration of diagnostic tests into different stages of the eradication campaign needs investigation. Finally, studies must be done to inform the optimum mass-treatment strategy for sustainable interruption of transmission.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mitjà, Oriol; Marks, Michael; Konan, Diby J. P.; Ayelo, Gilbert; Gonzalez-Beiras, Camila; Boua, Bernard (…); Asiedu, Kingsley B.
Global epidemiology of yaws: a systematic review Journal Article
In: The Lancet Global Health, vol. 3, no. 6, pp. e324-e331, 2015, ISSN: 2214-109X.
@article{Mitjà2015,
title = {Global epidemiology of yaws: a systematic review},
author = {Oriol Mitjà and Michael Marks and Diby J. P. Konan and Gilbert Ayelo and Camila Gonzalez-Beiras and Boua, Bernard (…) and Asiedu, Kingsley B. },
doi = {10.1016/S2214-109X(15)00011-X},
issn = {2214-109X},
year = {2015},
date = {2015-01-01},
urldate = {2015-01-01},
journal = {The Lancet Global Health},
volume = {3},
number = {6},
pages = {e324-e331},
publisher = {Elsevier},
abstract = {To achieve yaws eradication, the use of the new WHO strategy of initial mass treatment with azithromycin and surveillance twice a year needs to be extended everywhere the disease occurs. However, the geographic scope of the disease is unknown. We aimed to synthesise published and unpublished work to update the reported number of people with yaws at national and subnational levels and to estimate at-risk populations.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mitjà, Oriol; Lukehart, Sheila A.; Pokowas, Gideon; Moses, Penias; Kapa, August; Godornes, Charmie (…); Bassat, Quique.
Haemophilus ducreyi as a cause of skin ulcers in children from a yaws-endemic area of Papua New Guinea: a prospective cohort study Journal Article
In: The Lancet Global Health, vol. 2, no. 4, pp. e235-e241, 2014, ISSN: 2214-109X.
@article{Mitjà2014,
title = {Haemophilus ducreyi as a cause of skin ulcers in children from a yaws-endemic area of Papua New Guinea: a prospective cohort study},
author = {Oriol Mitjà and Sheila A. Lukehart and Gideon Pokowas and Penias Moses and August Kapa and Godornes, Charmie (…) and Bassat, Quique. },
doi = {10.1016/S2214-109X(14)70019-1},
issn = {2214-109X},
year = {2014},
date = {2014-01-01},
urldate = {2014-01-01},
journal = {The Lancet Global Health},
volume = {2},
number = {4},
pages = {e235-e241},
publisher = {Elsevier},
abstract = {Skin infections with ulceration are a major health problem in countries of the south Pacific region. Yaws, caused by Treponema pallidum subspecies pertenue and diagnosed by the presence of skin ulcers and a reactive syphilis serology, is one major cause, but this infection can be confused clinically with ulcers due to other causative agents. We investigated T pallidum pertenue and another bacterium known to cause skin infections in the Pacific islands emphHaemophilus ducreyi as causes of skin ulceration in a yaws-endemic region. Additionally, we identified specific signs and symptoms associated with these causative agents of cutaneous ulcers and compared these findings with laboratory-based diagnoses.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Ayove, Telek; Houniei, Wendy; Wangnapi, Regina; Bieb, Sibauk V.; Kazadi, Walter; Luke, Lisol-Nirau (…); Mitjà, Oriol.
Sensitivity and specificity of a rapid point-of-care test for active yaws: a comparative study Journal Article
In: The Lancet Global Health, vol. 2, no. 7, pp. e415-e421, 2014, ISSN: 2214-109X.
@article{Ayove2014,
title = {Sensitivity and specificity of a rapid point-of-care test for active yaws: a comparative study},
author = {Ayove, Telek and Houniei, Wendy and Wangnapi, Regina and Bieb, Sibauk V. and Kazadi, Walter and Luke, Lisol-Nirau (…) and Mitjà, Oriol.},
doi = {10.1016/S2214-109X(14)70231-1},
issn = {2214-109X},
year = {2014},
date = {2014-01-01},
urldate = {2014-01-01},
journal = {The Lancet Global Health},
volume = {2},
number = {7},
pages = {e415-e421},
publisher = {Elsevier},
abstract = {To eradicate yaws, national control programmes use the Morges strategy (initial mass treatment and biannual resurveys). The resurvey component is designed to actively detect and treat remaining yaws cases and is initiated on the basis of laboratory-supported reactive non-treponemal serology (using the rapid plasma reagin [RPR] test). Unfortunately, the RPR test is available rarely in yaws-endemic areas. We sought to assess a new point-of-care assay?the Dual Path Platform (DPP) syphilis assay, which is based on simultaneous detection of antibodies to treponemal and non-treponemal antigens?for guiding use of antibiotics for yaws eradication. A secondary goal was to ascertain at what timepoint the DPP assay line reverted to negative after treatment.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mitjà, Oriol; Asiedu, Kingsley; Mabey, David
Yaws Journal Article
In: The Lancet, vol. 381, no. 9868, pp. 763-773, 2013, ISSN: 0140-6736.
@article{Mitjà2013,
title = {Yaws},
author = {Oriol Mitjà and Kingsley Asiedu and David Mabey},
doi = {10.1016/S0140-6736(12)62130-8},
issn = {0140-6736},
year = {2013},
date = {2013-01-01},
journal = {The Lancet},
volume = {381},
number = {9868},
pages = {763-773},
publisher = {Elsevier},
abstract = {Yaws is an infectious disease caused by Treponema pallidum pertenue?a bacterium that closely resembles the causative agent of syphilis?and is spread by skin-to-skin contact in humid tropical regions. Yaws causes disfiguring, and sometimes painful lesions of the skin and bones. As with syphilis, clinical manifestations can be divided into three stages; however, unlike syphilis, mother-to-child transmission does not occur. A major campaign to eradicate yaws in the 1950s and 1960s, by mass treatment of affected communities with longacting, injectable penicillin, reduced the number of cases by 95% worldwide, but yaws has reappeared in recent years in Africa, Asia, and the western Pacific. In 2012, one oral dose of azithromycin was shown to be as effective as intramuscular penicillin in the treatment of the disease, and WHO launched a new initiative to eradicate yaws by 2020.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mitjà, Oriol; Hays, Russell; Ipai, Anthony; Penias, Moses; Paru, Raymond; Fagaho, David; Lazzari, Elisa; Bassat, Quique
In: The Lancet, vol. 379, no. 9813, pp. 342-347, 2012, ISSN: 0140-6736.
@article{Mitjà2012,
title = {Single-dose azithromycin versus benzathine benzylpenicillin for treatment of yaws in children in Papua New Guinea: an open-label, non-inferiority, randomised trial},
author = {Oriol Mitjà and Russell Hays and Anthony Ipai and Moses Penias and Raymond Paru and David Fagaho and Elisa Lazzari and Quique Bassat},
doi = {10.1016/S0140-6736(11)61624-3},
issn = {0140-6736},
year = {2012},
date = {2012-01-01},
journal = {The Lancet},
volume = {379},
number = {9813},
pages = {342-347},
publisher = {Elsevier},
abstract = {Yaws is an endemic treponematosis and, as such, a neglected tropical disease?is re-emerging in children in rural, tropical areas. Oral azithromycin is effective for syphilis. We assessed the efficacy of azithromycin compared with intramuscular long-acting penicillin to treat patients with yaws.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}