Global mpox outbreak

In May 2022, multiple outbreaks of infection by monkeypox were reported in non-endemic areas, such as Europe and the United States. Although monkeypox infection is not life-threatening, the rapid spread of the virus in areas without a history of community transmission raised the awareness of health authorities, which launched public health dictates for containing the outbreaks.
Early evidence tells us that monkeypox infection is behaving different than previous outbreaks. Based on the need to fully understand the infection to make evidence-based decisions on the public health control of the infection, we are working to contribute to the existing evidence gaps, such as transmission dynamics, clinical presentations, diagnostic tools, and vaccine response and immunology.
Publications
Mitjà, Oriol; Watson-Jones, Deborah; Choi, Edward M; Jalloh, Mohamed Boi; Sahr, Foday
Clade IIb mpox outbreak in Sierra Leone Journal Article
In: The Lancet, vol. 405, iss. 10497, pp. 2274-2275, 2025.
@article{nokey,
title = {Clade IIb mpox outbreak in Sierra Leone},
author = {Oriol Mitjà and Deborah Watson-Jones and Edward M Choi and Mohamed Boi Jalloh and Foday Sahr},
doi = {10.1016/S0140-6736(25)01203-6},
year = {2025},
date = {2025-06-20},
urldate = {2025-06-20},
journal = {The Lancet},
volume = {405},
issue = {10497},
pages = {2274-2275},
abstract = {The current mpox outbreak in Sierra Leone is the largest ever recorded in the country and the first major epidemic caused by the clade IIb monkeypox virus in Africa. Since a public health emergency was declared on Jan 13, 2025,1 3682 confirmed cases have been reported in Sierra Leone (as of June 4, 2025), with 2225 (60·4%) cases in Freetown (western urban), 748 (20·3%) cases in nearby suburban towns (western rural), and 709 (19·3%) cases distributed across the 14 other districts. Case numbers remained low throughout mid-April, but surged in late April (week 17) and throughout May, exceeding 600 confirmed cases weekly and indicating sustained transmission despite early signs of stabilisation (unpublished data).
The outbreak is mainly affecting young adults aged 20–34 years—including sex workers—and genital lesions are prevalent, suggesting substantial sexual transmission, as seen in clade IIb outbreaks in non-endemic countries since 2022 (unpublished data). Unlike those outbreaks, however, females and males are equally affected in Sierra Leone (47·5% female and 52·5% male). This pattern contrasts with historical clade IIb outbreaks in west Africa, which were typically small, zoonotic, and had little human-to-human spread.2 Instead, this outbreak resembles clade Ib outbreaks in DR Congo, Burundi, and Uganda,3,4 which were larger in scale, with broader geographical and demographic spread and similar rates of infection among females and males. This blurring of traditional clade-related phenotypes suggests that host, environmental, and social factors might be as determinant as viral genetics.2
Unpublished genomic sequencing of 77 samples by the Ministry of Health with regional and international partners5 shows a novel clade IIb lineage—A.2.2.1—derived from Nigerian A.2.2 viruses but forming a distinct monophyletic cluster, indicating local diversification. Bayesian analysis estimates the most recent common ancestor to be from mid-November, 2024, suggesting 1–2 months of undetected community transmission before the first confirmed case.5 High APOBEC3 mutation loads support ongoing human adaptation.
Clinical data from a preprint paper6 of 161 patients with probable or confirmed mpox show high rates of rash, fever, and generalised pain, with many patients also reporting lymphadenopathy, sore throat, and cough. Admission to hospital was required in 28·9% of patients, often due to disseminated lesions—particularly genital—again indicating sexual transmission.6
Vaccination began in Freetown and surrounding high-risk areas in March, 2025, targeting health-care workers, known contacts of people with confirmed disease, people living with HIV, military workers, and university students. As of June 4, 2025, more than 43 000 people have been vaccinated, but with only 80 000 doses delivered, the remaining doses are insufficient for large-scale vaccination (unpublished data). A new 400-bed mpox treatment centre is now operational in Freetown, but many patients still isolate at home due to low capacity and personal preference (unpublished data). The Government plans to open large-scale centres outside the capital. Contact tracing is nationwide, but situation reports show a declining number of listed contacts per patient with confirmed disease, likely due to rising caseloads and increasing strain on the system. Molecular testing is active at eight sites, with plans to expand (unpublished data).
Surveillance gaps likely contribute to under-reporting in rural areas. The Government has deployed rapid response teams and trained personnel for case investigation, and backlog data entry into the national health database continues. Community outreach and risk communication via radio, television, and targeted messaging is ongoing. The Africa Centres for Disease Control and Prevention have flagged the outbreak as a growing threat to the region.7 With Liberia reporting an increase in cases and with spillover effects in Togo and Ghana,4,7 the risk of cross-border spread is real. Genomic data have shown both viral imports and exports to and from Sierra Leone, including two sequences sampled in the USA and two in Germany,5 underscoring the need for coordinated surveillance, sequencing, and vaccine allocation across west Africa.
Accelerated vaccine delivery is urgently needed—not just in Sierra Leone, but across the region—to prevent wider dissemination of this evolving virus.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
The outbreak is mainly affecting young adults aged 20–34 years—including sex workers—and genital lesions are prevalent, suggesting substantial sexual transmission, as seen in clade IIb outbreaks in non-endemic countries since 2022 (unpublished data). Unlike those outbreaks, however, females and males are equally affected in Sierra Leone (47·5% female and 52·5% male). This pattern contrasts with historical clade IIb outbreaks in west Africa, which were typically small, zoonotic, and had little human-to-human spread.2 Instead, this outbreak resembles clade Ib outbreaks in DR Congo, Burundi, and Uganda,3,4 which were larger in scale, with broader geographical and demographic spread and similar rates of infection among females and males. This blurring of traditional clade-related phenotypes suggests that host, environmental, and social factors might be as determinant as viral genetics.2
Unpublished genomic sequencing of 77 samples by the Ministry of Health with regional and international partners5 shows a novel clade IIb lineage—A.2.2.1—derived from Nigerian A.2.2 viruses but forming a distinct monophyletic cluster, indicating local diversification. Bayesian analysis estimates the most recent common ancestor to be from mid-November, 2024, suggesting 1–2 months of undetected community transmission before the first confirmed case.5 High APOBEC3 mutation loads support ongoing human adaptation.
Clinical data from a preprint paper6 of 161 patients with probable or confirmed mpox show high rates of rash, fever, and generalised pain, with many patients also reporting lymphadenopathy, sore throat, and cough. Admission to hospital was required in 28·9% of patients, often due to disseminated lesions—particularly genital—again indicating sexual transmission.6
Vaccination began in Freetown and surrounding high-risk areas in March, 2025, targeting health-care workers, known contacts of people with confirmed disease, people living with HIV, military workers, and university students. As of June 4, 2025, more than 43 000 people have been vaccinated, but with only 80 000 doses delivered, the remaining doses are insufficient for large-scale vaccination (unpublished data). A new 400-bed mpox treatment centre is now operational in Freetown, but many patients still isolate at home due to low capacity and personal preference (unpublished data). The Government plans to open large-scale centres outside the capital. Contact tracing is nationwide, but situation reports show a declining number of listed contacts per patient with confirmed disease, likely due to rising caseloads and increasing strain on the system. Molecular testing is active at eight sites, with plans to expand (unpublished data).
Surveillance gaps likely contribute to under-reporting in rural areas. The Government has deployed rapid response teams and trained personnel for case investigation, and backlog data entry into the national health database continues. Community outreach and risk communication via radio, television, and targeted messaging is ongoing. The Africa Centres for Disease Control and Prevention have flagged the outbreak as a growing threat to the region.7 With Liberia reporting an increase in cases and with spillover effects in Togo and Ghana,4,7 the risk of cross-border spread is real. Genomic data have shown both viral imports and exports to and from Sierra Leone, including two sequences sampled in the USA and two in Germany,5 underscoring the need for coordinated surveillance, sequencing, and vaccine allocation across west Africa.
Accelerated vaccine delivery is urgently needed—not just in Sierra Leone, but across the region—to prevent wider dissemination of this evolving virus.
Suñer, Clara; Escrig-Sarreta, Roser; Galván-Casas, Cristina; Mateos, Eduardo; Gabster, Amanda; (…) Mitjà, Oriol
Target Trial Emulation of the Modified Vaccinia Ankara-Bavarian Nordic Vaccine for Pre-Exposure Mpox Prevention in At-Risk Populations Journal Article
In: Vaccines, vol. 13, iss. 6, 2025.
@article{nokey,
title = {Target Trial Emulation of the Modified Vaccinia Ankara-Bavarian Nordic Vaccine for Pre-Exposure Mpox Prevention in At-Risk Populations},
author = {Clara Suñer and Roser Escrig-Sarreta and Cristina Galván-Casas and Eduardo Mateos and Amanda Gabster and (…) Mitjà, Oriol},
doi = {10.3390/vaccines13060594},
year = {2025},
date = {2025-05-30},
urldate = {2025-05-30},
journal = {Vaccines},
volume = {13},
issue = {6},
abstract = {Background:The MVA-BN vaccine is considered effective for preventing mpox in key populations, based on observational studies, though no randomized trials have yet confirmed its effectiveness. Observational studies published to date rely on retrospective analyses of routine data, often missing information on relevant risk factors for mpox. Methods: Multi-country target trial emulation study with prospective data collection. Between 1 September 2022 and 15 June 2023, we recruited individuals eligible for mpox vaccination based on clinical history and exposure behaviors via healthcare centers and social venues in Spain, Peru, Panama, and Chile. Vaccinated individuals were paired with unvaccinated counterparts matched by mpox risk factors, country, recruitment date, and age. Follow-up continued via periodic surveys until 31 March 2024. The primary endpoint was symptomatic mpox occurrence ≥14 days post-vaccination. Results: The primary analysis included 1028 individuals (514 vaccinated, 514 unvaccinated) with a median follow-up time of 9.3 months (IQR 4.7–13.7). Mpox occurred in eight participants (0.8%): three vaccinated and five unvaccinated (HR 0.6; 95% CI 0.21–1.70). Adverse reactions were reported by 731 (49.6%) participants, predominantly skin reactions (703/1475; 47.7%), while systemic reactions occurred in 107 (7.3%). Long-lasting erythema at the injection site was reported in 450/1058 (42.5%) participants, persisting >6 months in 107 of them (23.8%). Conclusions: The low incidence of mpox during the study period resulted in a limited number of endpoint events, precluding robust conclusions on the efficacy of the MVA-BN vaccine as pre-exposure prevention for mpox. However, our analysis, which accounted for key confounders such as exposure behaviors, yielded results consistent with previous studies suggesting the effectiveness of the vaccine in the mpox setting.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Malembi, Emile; Escrig-Sarreta, Roser; Ntumba, Jackie; Shongo, Robert; Bengehya, Justin; (…) Mitjà, Oriol
Clinical presentation and epidemiological assessment of confirmed human mpox cases in DR Congo: a surveillance-based observational study Journal Article
In: The Lancet, vol. 405, iss. 10490, pp. 1666-1675, 2025.
@article{nokey,
title = {Clinical presentation and epidemiological assessment of confirmed human mpox cases in DR Congo: a surveillance-based observational study},
author = {Emile Malembi and Roser Escrig-Sarreta and Jackie Ntumba and Robert Shongo and Justin Bengehya and (…) Mitjà, Oriol},
doi = {10.1016/S0140-6736(25)00152-7},
year = {2025},
date = {2025-05-10},
urldate = {2025-05-10},
journal = {The Lancet},
volume = {405},
issue = {10490},
pages = {1666-1675},
abstract = {Background
Mpox, caused by the monkeypox virus, is a serious public health threat in Africa, especially in DR Congo. Previously limited to endemic areas with clade 1a, monkeypox virus has recently spread to non-endemic regions, where clade 1b has emerged. This study provides a clinical comparison of mpox cases in DR Congo regions where clade 1a and clade 1b are prevalent.
Methods
We conducted a retrospective observational study, analysing PCR-confirmed mpox cases reported from sentinel health zones in seven provinces between Oct 1, 2023, and Sept 31, 2024. Cases from the newly affected provinces (South-Kivu and Kinshasa) were described along with those from four endemic provinces (Mai-Ndombe, Tshuapa, Tshopo, South-Ubangi, and Équateur). Surveillance data, including type of exposure, demographic details, clinical presentation, complications, and outcomes were collected from national surveillance systems and local health facilities, with laboratory confirmation using quantitative PCR. All analyses were restricted to descriptive statistics.
Findings
Of 17 927 suspected cases identified, 10 986 were investigated, 5948 were PCR-positive, and 4895 met the inclusion criteria based on data completeness: 4436 in newly affected and 459 in endemic regions. In newly affected provinces, median age was 20 years (IQR 8–28), 2119 (47·8%) participants were female, and 2310 (52·1%) were male. In endemic provinces, median age was 15 years (7–26), 179 (39·0%) participants were female, and 277 (60·3%) were male. Direct or intimate human contact was reported by 1951 (44·0%) individuals in newly affected provinces versus 25 (5·4%) in endemic provinces, and zoonotic exposure in 11 (0·2%) and 99 (21·6%), respectively. The proportions of partcipants with systemic symptoms (3828 [86·3%] in newly affected provinces and 427 [93·0%] in endemic provinces) and respiratory symptoms (2450 [55·2%] and 219 [47·7%]), and median skin lesion counts (91 [IQR 37–200] and 163 [95–345]) were similar between newly affected and endemic regions. Complications included skin infections (2041 [46·0%] in newly affected provinces and 201 [43·8%] in endemic provinces), respiratory distress (82 [1·8%] and 29 [6·3%]), vision impairment (7 [0·2%] and 28 [6·1%]), and prostration (695 [15·7%] and 51 [11·1%]). The case-fatality rate was 0·7% (95% CI 0·4–1·3; 14 of 1924) in children and 0·6% (0·3–1·0; 14 of 2483) in adults in newly affected areas, compared with 5·9% (3·4–10·0; 14 of 236) in children and 2·7% (1·1–6·1; six of 222) in adults in endemic regions. Content note: this Article and its appendix contain graphic images of mpox lesions affecting various sites including the face and genitals.
Interpretation
Our study indicates concurrent mpox outbreaks in DR Congo, involving younger individuals, a higher proportion of women and girls, and distinct presentations with higher lesion counts and respiratory symptoms compared with clade 2b lineage B.1 outbreaks. The high proportion of infectious complications and case-fatality rates, especially in endemic regions, emphasise the need for timely antibiotic therapy and targeted vaccination to reduce morbidity and mortality.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mpox, caused by the monkeypox virus, is a serious public health threat in Africa, especially in DR Congo. Previously limited to endemic areas with clade 1a, monkeypox virus has recently spread to non-endemic regions, where clade 1b has emerged. This study provides a clinical comparison of mpox cases in DR Congo regions where clade 1a and clade 1b are prevalent.
Methods
We conducted a retrospective observational study, analysing PCR-confirmed mpox cases reported from sentinel health zones in seven provinces between Oct 1, 2023, and Sept 31, 2024. Cases from the newly affected provinces (South-Kivu and Kinshasa) were described along with those from four endemic provinces (Mai-Ndombe, Tshuapa, Tshopo, South-Ubangi, and Équateur). Surveillance data, including type of exposure, demographic details, clinical presentation, complications, and outcomes were collected from national surveillance systems and local health facilities, with laboratory confirmation using quantitative PCR. All analyses were restricted to descriptive statistics.
Findings
Of 17 927 suspected cases identified, 10 986 were investigated, 5948 were PCR-positive, and 4895 met the inclusion criteria based on data completeness: 4436 in newly affected and 459 in endemic regions. In newly affected provinces, median age was 20 years (IQR 8–28), 2119 (47·8%) participants were female, and 2310 (52·1%) were male. In endemic provinces, median age was 15 years (7–26), 179 (39·0%) participants were female, and 277 (60·3%) were male. Direct or intimate human contact was reported by 1951 (44·0%) individuals in newly affected provinces versus 25 (5·4%) in endemic provinces, and zoonotic exposure in 11 (0·2%) and 99 (21·6%), respectively. The proportions of partcipants with systemic symptoms (3828 [86·3%] in newly affected provinces and 427 [93·0%] in endemic provinces) and respiratory symptoms (2450 [55·2%] and 219 [47·7%]), and median skin lesion counts (91 [IQR 37–200] and 163 [95–345]) were similar between newly affected and endemic regions. Complications included skin infections (2041 [46·0%] in newly affected provinces and 201 [43·8%] in endemic provinces), respiratory distress (82 [1·8%] and 29 [6·3%]), vision impairment (7 [0·2%] and 28 [6·1%]), and prostration (695 [15·7%] and 51 [11·1%]). The case-fatality rate was 0·7% (95% CI 0·4–1·3; 14 of 1924) in children and 0·6% (0·3–1·0; 14 of 2483) in adults in newly affected areas, compared with 5·9% (3·4–10·0; 14 of 236) in children and 2·7% (1·1–6·1; six of 222) in adults in endemic regions. Content note: this Article and its appendix contain graphic images of mpox lesions affecting various sites including the face and genitals.
Interpretation
Our study indicates concurrent mpox outbreaks in DR Congo, involving younger individuals, a higher proportion of women and girls, and distinct presentations with higher lesion counts and respiratory symptoms compared with clade 2b lineage B.1 outbreaks. The high proportion of infectious complications and case-fatality rates, especially in endemic regions, emphasise the need for timely antibiotic therapy and targeted vaccination to reduce morbidity and mortality.
Gonzalez-Beiras, Camila; Malembi, Emile; Escrig-Sarreta, Roser; Ahuka, Steve; Mbala, Placide; Mavoko, Hypolite (…); Mitjà, Oriol
Concurrent outbreaks of mpox in Africa—an update Journal Article
In: The Lancet, vol. 405, iss. 10472, 2025.
@article{nokey,
title = {Concurrent outbreaks of mpox in Africa—an update},
author = {Camila Gonzalez-Beiras and Emile Malembi and Roser Escrig-Sarreta and Steve Ahuka and Placide Mbala and Mavoko, Hypolite (…) and Mitjà, Oriol},
doi = {10.1016/S0140-6736(24)02353-5},
year = {2025},
date = {2025-01-04},
urldate = {2025-01-04},
journal = {The Lancet},
volume = {405},
issue = {10472},
abstract = {In this Review, we examine the concurrent outbreaks of mpox in Africa, focusing on clade 1a, the newly emerged clade 1b, and clade 2b lineage A, and how they differ from the 2022 global outbreak caused by clade 2b lineage B.1. Historically, clades 1a and 2a have caused sporadic, small outbreaks in central and west Africa, respectively, primarily through zoonotic transmission. Clade 2b first caused an outbreak in Nigeria in 2017, and later spread globally via sexual contact in 2022. In August, 2024, WHO declared a global health emergency due to the newly identified clade 1b outbreak in eastern Democratic Republic of the Congo. This outbreak has now expanded to several other countries and is spreading through direct and sexual contact in urban centres and refugee camps. Clades, route of exposure, infectious dose, and host immune response are the main factors influencing clinical presentation of mpox. For clades 1a and 2a, zoonotic transmission plays an important role, whereas for clades 1b and 2b, the spread occurs through sustained human-to-human transmission without zoonotic exposure. For both clades 1a and 2a, lesions have a generalised centrifugal distribution, whereas for clade 2b they are mainly localised to the anogenital area. For clade 1b, data are still emerging, but current cases show a mix of localised lesions and centrifugal distribution. The severity of the disease is higher for clade 1a (case fatality rate up to 12%) compared with other clades (case fatality rates 0–3·6%). Diagnostic challenges include false negative results for clade 1b with existing PCR assays and poor testing access in remote areas. Tecovirimat, the primary antiviral during the 2022 outbreak, has shown reduced effectiveness against clade 1a in preliminary study results, whereas its efficacy against other clades is still under investigation. The modified vaccinia Ankara–Bavarian Nordic vaccine has been shown to be up to 90% effective against clade 2b after two doses and is safe for children, although its effectiveness drops to 20% when used as post-exposure prophylaxis. Given the evolving nature of the monkeypox virus, ongoing research and strong public health responses are key to managing potential future outbreaks.
},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Moraes Cardoso, Igor; Benet, Susana; Carabelli, Julieta; Perez-Zsolt, Daniel; Mendoza, Adrià; Rivero, Angel (…); Mothe, Beatriz
Immune responses associated with mpox viral clearance in men with and without HIV in Spain: a multisite, observational, prospective cohort study Journal Article
In: The Lancet Microbe , vol. 5, iss. 18, 2024.
@article{nokey,
title = {Immune responses associated with mpox viral clearance in men with and without HIV in Spain: a multisite, observational, prospective cohort study},
author = {Moraes Cardoso, Igor and Benet, Susana and Carabelli, Julieta and Perez-Zsolt, Daniel and Mendoza, Adrià and Rivero, Angel (…) and Mothe, Beatriz},
doi = {10.1016/S2666-5247(24)00074-0 },
year = {2024},
date = {2024-08-09},
urldate = {2024-08-09},
journal = {The Lancet Microbe },
volume = {5},
issue = {18},
abstract = {Background
Since the emergence of the global mpox outbreak in May, 2022, more than 90 000 cases have been diagnosed across 110 countries, disproportionately affecting people with HIV. The durability of mpox-specific immunity is unclear and reinfections have been reported. We aimed to compare mpox immune responses up to 6 months after diagnosis in participants with and without HIV and assess their effect on disease severity and viral clearance dynamics.
Methods
This study was embedded within a prospective, observational, multicentre cohort study of viral clearance dynamics among people with mpox in Spain (MoViE). We included women and men aged 18 years or older, who had signs of mpox, and reported having symptom onset within the previous 10 days at the moment of mpox diagnosis from three sex clinics of the Barcelona metropolitan area. Samples from skin ulcers were collected weekly to estimate the time to clear monkeypox virus (MPXV) from skin lesions. Blood samples were taken at diagnosis, 29, 91, and 182 days later for immune analysis. This included quantifying IgG and IgA against three mpox antigens by ELISA, evaluating in-vitro neutralisation, and characterising mpox-specific T-cell responses using interferon γ detecting enzyme-linked immunospot (ELISpot) assay and multiparametric flow cytometry.
Findings
Of the 77 originally enrolled participants, we included 33 participants recruited between July 19, and Oct 6, 2022. Participants without HIV (19 [58%] participants) and participants with HIV (14 [42%] participants) had similar clinical severity and time to MPXV clearance in skin lesions. Participants with HIV had a CD4+ T-cell count median of 777 cells per μL (IQR 484–1533), and 11 (78%) of 14 were virally suppressed on antiretroviral therapy. Nine (27%) of 33 participants were age 49 years or older. 15 (45%) of 33 participants were originally from Spain, and all participants were men. Early humoral responses, particularly concentrations and breadth of IgG and IgA, were associated with milder disease and faster viral clearance. Orthopoxvirus-specific T cells count was also positively correlated with MPXV clearance. Antibody titres declined more rapidly in participants with HIV, but T-cell responses against MPXV were sustained up to day 182 after diagnosis, regardless of HIV status.
Interpretation
Higher breadth and magnitude of B-cell and T-cell responses are important in facilitating local viral clearance, limiting mpox dissemination, and reducing disease severity in individuals with preserved immune system. Antibodies appear to contribute to early viral control and T-cell responses are sustained over time, which might contribute to milder presentations during reinfection.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Since the emergence of the global mpox outbreak in May, 2022, more than 90 000 cases have been diagnosed across 110 countries, disproportionately affecting people with HIV. The durability of mpox-specific immunity is unclear and reinfections have been reported. We aimed to compare mpox immune responses up to 6 months after diagnosis in participants with and without HIV and assess their effect on disease severity and viral clearance dynamics.
Methods
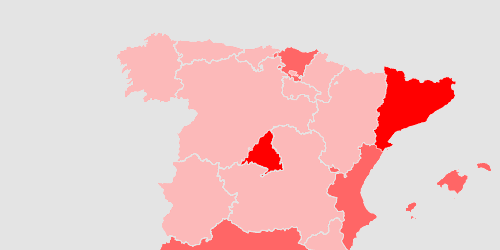
This study was embedded within a prospective, observational, multicentre cohort study of viral clearance dynamics among people with mpox in Spain (MoViE). We included women and men aged 18 years or older, who had signs of mpox, and reported having symptom onset within the previous 10 days at the moment of mpox diagnosis from three sex clinics of the Barcelona metropolitan area. Samples from skin ulcers were collected weekly to estimate the time to clear monkeypox virus (MPXV) from skin lesions. Blood samples were taken at diagnosis, 29, 91, and 182 days later for immune analysis. This included quantifying IgG and IgA against three mpox antigens by ELISA, evaluating in-vitro neutralisation, and characterising mpox-specific T-cell responses using interferon γ detecting enzyme-linked immunospot (ELISpot) assay and multiparametric flow cytometry.
Findings
Of the 77 originally enrolled participants, we included 33 participants recruited between July 19, and Oct 6, 2022. Participants without HIV (19 [58%] participants) and participants with HIV (14 [42%] participants) had similar clinical severity and time to MPXV clearance in skin lesions. Participants with HIV had a CD4+ T-cell count median of 777 cells per μL (IQR 484–1533), and 11 (78%) of 14 were virally suppressed on antiretroviral therapy. Nine (27%) of 33 participants were age 49 years or older. 15 (45%) of 33 participants were originally from Spain, and all participants were men. Early humoral responses, particularly concentrations and breadth of IgG and IgA, were associated with milder disease and faster viral clearance. Orthopoxvirus-specific T cells count was also positively correlated with MPXV clearance. Antibody titres declined more rapidly in participants with HIV, but T-cell responses against MPXV were sustained up to day 182 after diagnosis, regardless of HIV status.
Interpretation
Higher breadth and magnitude of B-cell and T-cell responses are important in facilitating local viral clearance, limiting mpox dissemination, and reducing disease severity in individuals with preserved immune system. Antibodies appear to contribute to early viral control and T-cell responses are sustained over time, which might contribute to milder presentations during reinfection.
Hazra, Aniruddha; Zucker, Jason; Bell, Elizabeth; Flores, John; Gordon, Leanna; Mitjà, Oriol (…); Orkin, Chloe
Mpox in people with past infection or a complete vaccination course: a global case series Journal Article
In: The Lancet Infectious Diseases, vol. 24, iss. 1, 2024.
@article{nokey,
title = {Mpox in people with past infection or a complete vaccination course: a global case series},
author = {Aniruddha Hazra and Jason Zucker and Elizabeth Bell and John Flores and Leanna Gordon and Mitjà, Oriol (…) and Chloe Orkin},
doi = {10.1016/S1473-3099(23)00492-9},
year = {2024},
date = {2024-01-22},
urldate = {2024-01-22},
journal = {The Lancet Infectious Diseases},
volume = {24},
issue = {1},
abstract = {Background: Since May, 2022, a large global outbreak of human mpox (formerly known as monkeypox) has predominantly affected men who have sex with men. The strain responsible, Clade IIb, has mutated substantially from precursors originating from the 2017-18 outbreak in Nigeria. Immunity to smallpox, another orthopoxvirus, via previous infection or vaccination provides lifelong immunity. However, since the 2022 mpox outbreak, recent clusters were described in individuals with presumed immunity through recent infection or vaccination. We aim to describe the epidemiological and clinical characteristics of mpox in individuals with past infection or vaccination to improve the understanding of this disease in the setting of previous immunity.
Methods: In this global case series, international collaborators from nine countries provided data on individuals with PCR-confirmed mpox after documented previous infection or vaccination between May 11, 2022, and June 30, 2023. We excluded cases that could not confirm vaccination status or cases with partial immunisation or any doses received before the current multi-national mpox outbreak (cutoff date May 1, 2022). Data were collected via a case report spreadsheet that reported on dates of infection and vaccination, route of immunisation, demographic characteristics, clinical findings, HIV status, concomitant sexually transmitted infections, and markers of disease severity (mpox severity score system). We describe case epidemiology, clinical course, and mpox severity scores; all analyses were descriptive.
Findings: We report mpox infections in 37 gay and bisexual men who have sex with men: seven individuals had mpox reinfections, 29 individuals had mpox infections that occurred after two appropriately spaced Modified Vaccinia Ankara-Bavarian Nordic vaccine courses, and one individual had an infection that met the criteria for both reinfection and infection after vaccination. The median age of individuals was 36 years (IQR 30-45; range 21-58). Those with natural immunity after initial infection had a shorter disease course with less mucosal disease upon reinfection than with their initial infection. Infections post-vaccination were characterised by few lesions, little mucosal disease, and minimal analgesia requirements; two people received oral tecovirimat. Overall, there were no deaths, no bacterial superinfections, and all individuals were managed in the ambulatory clinic with one hospital admission for a necrotising neck lesion.
Interpretation: The epidemiology of people with mpox reinfection or infection post-vaccination was similar to other published cohorts during the 2022 outbreak-predominantly young, sexually active gay and bisexual men who have sex with men. Clinical features and outcomes of repeat infection and infection after vaccination appear to be less clinically severe than those described in 2022 case literature. Specifically, compared with the 2022 case series, these individuals in the present study had fewer confluent lesions, less mucosal involvement, reduced analgesia requirement, and fewer admissions. Natural immunity and vaccine-induced immunity are not fully protective against mpox infection. However, in this small series both disease duration and severity appear to be reduced.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Methods: In this global case series, international collaborators from nine countries provided data on individuals with PCR-confirmed mpox after documented previous infection or vaccination between May 11, 2022, and June 30, 2023. We excluded cases that could not confirm vaccination status or cases with partial immunisation or any doses received before the current multi-national mpox outbreak (cutoff date May 1, 2022). Data were collected via a case report spreadsheet that reported on dates of infection and vaccination, route of immunisation, demographic characteristics, clinical findings, HIV status, concomitant sexually transmitted infections, and markers of disease severity (mpox severity score system). We describe case epidemiology, clinical course, and mpox severity scores; all analyses were descriptive.
Findings: We report mpox infections in 37 gay and bisexual men who have sex with men: seven individuals had mpox reinfections, 29 individuals had mpox infections that occurred after two appropriately spaced Modified Vaccinia Ankara-Bavarian Nordic vaccine courses, and one individual had an infection that met the criteria for both reinfection and infection after vaccination. The median age of individuals was 36 years (IQR 30-45; range 21-58). Those with natural immunity after initial infection had a shorter disease course with less mucosal disease upon reinfection than with their initial infection. Infections post-vaccination were characterised by few lesions, little mucosal disease, and minimal analgesia requirements; two people received oral tecovirimat. Overall, there were no deaths, no bacterial superinfections, and all individuals were managed in the ambulatory clinic with one hospital admission for a necrotising neck lesion.
Interpretation: The epidemiology of people with mpox reinfection or infection post-vaccination was similar to other published cohorts during the 2022 outbreak-predominantly young, sexually active gay and bisexual men who have sex with men. Clinical features and outcomes of repeat infection and infection after vaccination appear to be less clinically severe than those described in 2022 case literature. Specifically, compared with the 2022 case series, these individuals in the present study had fewer confluent lesions, less mucosal involvement, reduced analgesia requirement, and fewer admissions. Natural immunity and vaccine-induced immunity are not fully protective against mpox infection. However, in this small series both disease duration and severity appear to be reduced.
Sonmez, Ibrahim; Martínez Riveros, Héctor; Folch, Cinta; Suñer, Clara; Diaz, Yesika; Alonso, Lucía; (…) Casabona, Jordi
Egocentric sexual network analysis among gay and bisexual men who have sex with men with and without mpox infection Journal Article
In: Sexually Transmitted Infections, vol. 99, iss. 8, 2023.
@article{nokey,
title = {Egocentric sexual network analysis among gay and bisexual men who have sex with men with and without mpox infection},
author = {Sonmez, Ibrahim and Martínez Riveros, Héctor and Cinta Folch and Clara Suñer and Yesika Diaz and Lucía Alonso and (…) Casabona, Jordi},
doi = {10.1136/sextrans-2023-055901},
year = {2023},
date = {2023-12-13},
urldate = {2023-12-13},
journal = {Sexually Transmitted Infections},
volume = {99},
issue = {8},
abstract = {Objectives: Recent outbreaks of the mpox (monkeypox) virus have been detected in dense sexual networks of gay and bisexual men who have sex with men (GBMSM). The objective of this study is to describe and compare the epidemiological and behavioural characteristics, as well as the sexual networks, of GBMSM diagnosed with mild mpox in Spain.
Methods: A prospective case-control study was conducted in Spain from July 2022 to February 2023. The study targeted a key population of GBMSM aged 18 years or older. Study participants were categorised into cases, those who were diagnosed with mpox virus infection; and controls, those who were not diagnosed. We examined and compared the sexual network characteristics of the two groups-mpox-positive (mpox-P) and mpox-negative (mpox-N) egos-using χ2, t-test and Wilcoxon test to examine the differences between the two groups in each section. Finally, we conducted univariable and multivariable logistic regressions to determine the factors associated with mpox infection.
Results: Among the 105 participants, 35 (33.3%) were mpox-P. Compared with mpox-N, mpox-P respondents more frequently reported syphilis (mpox-P: 31.4%; mpox-N: 12.9%) and HIV (mpox-P: 45.7%; mpox-N: 18.6%), and mpox-P individuals to have had at least one sexual contact with a confirmed mpox case (mpox-P: 62.5%; mpox-N: 8.3%). In the egocentric network analysis, mpox-P respondents had a higher prevalence of group sex with alters (mpox-P: 18.5%; mpox-N: 8.9%) and one-time sexual partners (mpox-P: 46.1%; mpox-N: 31.7%). Multivariable logistic regressions showed that reporting stranger/client ties (adjusted OR (aOR)=10.3, 95% CI 1.39 to 76.6) with alters, being vaccinated for mpox (aOR=0.07, 95% CI 0.02 to 0.24) and tie strength heterogeneity (aOR=0.01, 95% CI 0.00 to 0.42) were associated with mpox infection.
Conclusions: Our findings highlight the role of demographic, epidemiological and sexual network characteristics in the transmission of mpox virus during the outbreak in Spain. These findings have important implications for future prevention efforts.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Methods: A prospective case-control study was conducted in Spain from July 2022 to February 2023. The study targeted a key population of GBMSM aged 18 years or older. Study participants were categorised into cases, those who were diagnosed with mpox virus infection; and controls, those who were not diagnosed. We examined and compared the sexual network characteristics of the two groups-mpox-positive (mpox-P) and mpox-negative (mpox-N) egos-using χ2, t-test and Wilcoxon test to examine the differences between the two groups in each section. Finally, we conducted univariable and multivariable logistic regressions to determine the factors associated with mpox infection.
Results: Among the 105 participants, 35 (33.3%) were mpox-P. Compared with mpox-N, mpox-P respondents more frequently reported syphilis (mpox-P: 31.4%; mpox-N: 12.9%) and HIV (mpox-P: 45.7%; mpox-N: 18.6%), and mpox-P individuals to have had at least one sexual contact with a confirmed mpox case (mpox-P: 62.5%; mpox-N: 8.3%). In the egocentric network analysis, mpox-P respondents had a higher prevalence of group sex with alters (mpox-P: 18.5%; mpox-N: 8.9%) and one-time sexual partners (mpox-P: 46.1%; mpox-N: 31.7%). Multivariable logistic regressions showed that reporting stranger/client ties (adjusted OR (aOR)=10.3, 95% CI 1.39 to 76.6) with alters, being vaccinated for mpox (aOR=0.07, 95% CI 0.02 to 0.24) and tie strength heterogeneity (aOR=0.01, 95% CI 0.00 to 0.42) were associated with mpox infection.
Conclusions: Our findings highlight the role of demographic, epidemiological and sexual network characteristics in the transmission of mpox virus during the outbreak in Spain. These findings have important implications for future prevention efforts.
Ubals, Maria; Tarín-Vicente, Eloy José; Oller, Xènia; Mendoza, Adrià; Alemany, Andrea; Hernández-Rodríguez, Águeda (…); Mitjà, Oriol.
Evaluating the accuracy of self-collected swabs for the diagnoss of monkeypox Journal Article
In: Clinical Infectious Diseases, vol. 7, no. 76, pp. 1311-1314, 2023, ISBN: 1537-6591.
@article{Ubals2022-tf,
title = {Evaluating the accuracy of self-collected swabs for the diagnoss of monkeypox},
author = {Ubals, Maria and Tarín-Vicente, Eloy José and Oller, Xènia and Mendoza, Adrià and Alemany, Andrea and Hernández-Rodríguez, Águeda (…) and Mitjà, Oriol.},
doi = {10.1093/cid/ciac889},
isbn = {1537-6591},
year = {2023},
date = {2023-04-03},
urldate = {2023-04-03},
journal = {Clinical Infectious Diseases},
volume = {7},
number = {76},
pages = {1311-1314},
abstract = {We evaluated the accuracy of patient-collected skin lesions, oropharyngeal, and rectal swabs among 50 individuals enrolled in a study of mpox viral dynamics. We found that the performance of self-collected samples was similar to that of physician-collected samples, suggesting that self-sampling is a reliable strategy for diagnosing mpox.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mitjà, Oriol; Alemany, Andrea; Marks, Michael; Lezama Mora, Jezer; Rodríguez-Aldama, Juan Carlos; Torres, Mayara (…); Villareal, Diana.
Mpox in people with advanced HIV infection: a global case series Journal Article
In: The Lancet, 2023, ISSN: 0140-6736.
@article{monki,
title = {Mpox in people with advanced HIV infection: a global case series},
author = {Mitjà, Oriol and Alemany, Andrea and Marks, Michael and Lezama Mora, Jezer and Rodríguez-Aldama, Juan Carlos and Torres, Mayara (…) and Villareal, Diana.},
doi = {https://doi.org/10.1016/S0140-6736(23)00273-8},
issn = {0140-6736},
year = {2023},
date = {2023-01-01},
urldate = {2023-01-01},
journal = {The Lancet},
publisher = {Elsevier},
abstract = {BackgroundPeople living with HIV have accounted for 38?50% of those affected in the 2022 multicountry mpox outbreak. Most reported cases were in people who had high CD4 cell counts and similar outcomes to those without HIV. Emerging data suggest worse clinical outcomes and higher mortality in people with more advanced HIV. We describe the clinical characteristics and outcomes of mpox in a cohort of people with HIV and low CD4 cell counts (CD4 <350 cells per mm3).},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Suñer, Clara; Ubals, Maria; Tarín-Vicente, Eloy José; Mendoza, Adrià; Alemany, Andrea; Hernández-Rodríguez, Agueda (…); Mitjà, Oriol.
Viral dynamics in patients with monkeypox infection: a prospective cohort study in Spain Journal Article
In: The Lancet Infectious Diseases, 2023, ISSN: 1473-3099.
@article{sunyer2023,
title = {Viral dynamics in patients with monkeypox infection: a prospective cohort study in Spain},
author = {Suñer, Clara and Ubals, Maria and Tarín-Vicente, Eloy José and Mendoza, Adrià and Alemany, Andrea and Hernández-Rodríguez, Agueda (…) and Mitjà, Oriol.},
doi = {https://doi.org/10.1016/S1473-3099(22)00794-0},
issn = {1473-3099},
year = {2023},
date = {2023-01-01},
urldate = {2023-01-01},
journal = {The Lancet Infectious Diseases},
publisher = {Elsevier},
abstract = {BackgroundMonkeypox DNA has been detected in skin lesions, saliva, oropharynx, urine, semen, and stool of patients infected during the 2022 clade IIb outbreak; however, the viral dynamics within these compartments remain unknown. We aimed to characterise the viral load kinetics over time in various parts of the body.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Thornhill, John P; Palich, Romain; Ghosn, Jade; Walmsley, Sharon; Moschese, Davide; Cortes, Claudia P (…); Orkin, Chloe
Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series Journal Article
In: The Lancet, vol. 400, iss. 10367, pp. 1953-1965, 2022.
@article{nokey,
title = {Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series},
author = {John P Thornhill and Romain Palich and Jade Ghosn and Sharon Walmsley and Davide Moschese and Cortes, Claudia P (…) and Orkin, Chloe},
doi = {10.1016/S0140-6736(22)02187-0},
year = {2022},
date = {2022-12-03},
journal = {The Lancet},
volume = {400},
issue = {10367},
pages = {1953-1965},
abstract = {Background
Between May and November, 2022, global outbreaks of human monkeypox virus infection have been reported in more than 78 000 people worldwide, predominantly in men who have sex with men. We describe the epidemiological and clinical characteristics of monkeypox virus infection in cisgender (cis) and transgender (trans) women and non-binary individuals assigned female sex at birth to improve identification and understanding of risk factors.
Methods
International collaborators in geographical locations with high numbers of diagnoses of monkeypox virus infection were approached and invited to contribute data on women and non-binary individuals with confirmed monkeypox virus infection. Contributing centres completed deidentified structured case-report spreadsheets, adapted and developed by participating clinicians, to include variables of interest relevant to women and non-binary individuals assigned female at birth. We describe the epidemiology and clinical course observed in the reported infections.
Findings
Collaborators reported data for a total of 136 individuals with monkeypox virus infection who presented between May 11 and Oct 4, 2022, across 15 countries. Overall median age was 34 years (IQR 28–40; range 19–84). The cohort comprised 62 trans women, 69 cis women, and five non-binary individuals (who were, because of small numbers, grouped with cis women to form a category of people assigned female at birth for the purpose of comparison). 121 (89%) of 136 individuals reported sex with men. 37 (27%) of all individuals were living with HIV, with a higher proportion among trans women (31 [50%] of 62) than among cis women and non-binary individuals (six [8%] of 74). Sexual transmission was suspected in 55 (89%) trans women (with the remainder having an unknown route of transmission) and 45 (61%) cis women and non-binary individuals; non-sexual routes of transmission (including household and occupational exposures) were reported only in cis women and non-binary individuals. 25 (34%) of 74 cis women and non-binary individuals submitted to the case series were initially misdiagnosed. Overall, among individuals with available data, rash was described in 124 (93%) of 134 individuals and described as anogenital in 95 (74%) of 129 and as vesiculopustular in 105 (87%) of 121. Median number of lesions was ten (IQR 5-24; range 1–200). Mucosal lesions involving the vagina, anus, or oropharynx or eye occurred in 65 (55%) of 119 individuals with available data. Vaginal and anal sex were associated with lesions at those sites. Monkeypox virus DNA was detected by PCR from vaginal swab samples in all 14 samples tested. 17 (13%) individuals were hospitalised, predominantly for bacterial superinfection of lesions and pain management. 33 (24%) individuals were treated with tecovirimat and six (4%) received post-exposure vaccinations. No deaths were reported.
Interpretation
The clinical features of monkeypox in women and non-binary individuals were similar to those described in men, including the presence of anal and genital lesions with prominent mucosal involvement. Anatomically, anogenital lesions were reflective of sexual practices: vulvovaginal lesions predominated in cis women and non-binary individuals and anorectal features predominated in trans women. The prevalence of HIV co-infection in the cohort was high.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Between May and November, 2022, global outbreaks of human monkeypox virus infection have been reported in more than 78 000 people worldwide, predominantly in men who have sex with men. We describe the epidemiological and clinical characteristics of monkeypox virus infection in cisgender (cis) and transgender (trans) women and non-binary individuals assigned female sex at birth to improve identification and understanding of risk factors.
Methods
International collaborators in geographical locations with high numbers of diagnoses of monkeypox virus infection were approached and invited to contribute data on women and non-binary individuals with confirmed monkeypox virus infection. Contributing centres completed deidentified structured case-report spreadsheets, adapted and developed by participating clinicians, to include variables of interest relevant to women and non-binary individuals assigned female at birth. We describe the epidemiology and clinical course observed in the reported infections.
Findings
Collaborators reported data for a total of 136 individuals with monkeypox virus infection who presented between May 11 and Oct 4, 2022, across 15 countries. Overall median age was 34 years (IQR 28–40; range 19–84). The cohort comprised 62 trans women, 69 cis women, and five non-binary individuals (who were, because of small numbers, grouped with cis women to form a category of people assigned female at birth for the purpose of comparison). 121 (89%) of 136 individuals reported sex with men. 37 (27%) of all individuals were living with HIV, with a higher proportion among trans women (31 [50%] of 62) than among cis women and non-binary individuals (six [8%] of 74). Sexual transmission was suspected in 55 (89%) trans women (with the remainder having an unknown route of transmission) and 45 (61%) cis women and non-binary individuals; non-sexual routes of transmission (including household and occupational exposures) were reported only in cis women and non-binary individuals. 25 (34%) of 74 cis women and non-binary individuals submitted to the case series were initially misdiagnosed. Overall, among individuals with available data, rash was described in 124 (93%) of 134 individuals and described as anogenital in 95 (74%) of 129 and as vesiculopustular in 105 (87%) of 121. Median number of lesions was ten (IQR 5-24; range 1–200). Mucosal lesions involving the vagina, anus, or oropharynx or eye occurred in 65 (55%) of 119 individuals with available data. Vaginal and anal sex were associated with lesions at those sites. Monkeypox virus DNA was detected by PCR from vaginal swab samples in all 14 samples tested. 17 (13%) individuals were hospitalised, predominantly for bacterial superinfection of lesions and pain management. 33 (24%) individuals were treated with tecovirimat and six (4%) received post-exposure vaccinations. No deaths were reported.
Interpretation
The clinical features of monkeypox in women and non-binary individuals were similar to those described in men, including the presence of anal and genital lesions with prominent mucosal involvement. Anatomically, anogenital lesions were reflective of sexual practices: vulvovaginal lesions predominated in cis women and non-binary individuals and anorectal features predominated in trans women. The prevalence of HIV co-infection in the cohort was high.
Tarín-Vicente, Eloy José; Alemany, Andrea; Agud-Dios, Manuel; Ubals, Maria; Suñer, Clara; Antón, Andrés (…); Mitjà, Oriol.
Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study Journal Article
In: The Lancet, vol. 400, no. 10353, pp. 661-669, 2022, ISSN: 0140-6736.
@article{Tarín-Vicente2022,
title = {Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study},
author = {Tarín-Vicente, Eloy José and Alemany, Andrea and Agud-Dios, Manuel and Ubals, Maria and Suñer, Clara and Antón, Andrés (…) and Mitjà, Oriol.},
doi = {https://doi.org/10.1016/S0140-6736(22)01436-2},
issn = {0140-6736},
year = {2022},
date = {2022-01-01},
urldate = {2022-01-01},
journal = {The Lancet},
volume = {400},
number = {10353},
pages = {661-669},
publisher = {Elsevier},
abstract = {In May, 2022, several European countries reported autochthonous cases of monkeypox, which rapidly spread globally. Early reports suggest atypical presentations. We aimed to investigate clinical and virological characteristics of cases of human monkeypox in Spain.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Mitjà, Oriol; Ogoina, Dimie; Titanji, Boghuma K.; Galvan, Cristina; Muyembe, Jean-Jacques; Marks, Michael; Orkin, Chloe M.
Monkeypox Journal Article
In: The Lancet, 2022, ISSN: 0140-6736.
@article{ref1_mitjas,
title = {Monkeypox},
author = {Oriol Mitjà and Dimie Ogoina and Boghuma K. Titanji and Cristina Galvan and Jean-Jacques Muyembe and Michael Marks and Chloe M. Orkin},
doi = {https://doi.org/10.1016/S0140-6736(22)02075-X},
issn = {0140-6736},
year = {2022},
date = {2022-01-01},
journal = {The Lancet},
publisher = {Elsevier},
abstract = {Monkeypox is a zoonotic illness caused by the monkeypox virus, an Orthopoxvirus in the same genus as the variola, vaccinia, and cowpox viruses. Since the detection of the first human case in the Democratic Republic of the Congo in 1970, the disease has caused sporadic infections and outbreaks, mainly restricted to some countries in west and central Africa. In July, 2022, WHO declared monkeypox a Public Health Emergency of International Concern, on account of the unprecedented global spread of the disease outside previously endemic countries in Africa and the need for global solidarity to address this previously neglected disease. The 2022 outbreak has been primarily associated with close intimate contact (including sexual activity) and most cases have been diagnosed among men who have sex with men, who often present with novel epidemiological and clinical characteristics. In the 2022 outbreak, the incubation period ranges from 7 days to 10 days and most patients present with a systemic illness that includes fever and myalgia and a characteristic rash, with papules that evolve to vesicles, pustules, and crusts in the genital, anal, or oral regions and often involve the mucosa. Complications that require medical treatment (eg, antiviral therapy, antibacterials, and pain control) occur in up to 40% of patients and include rectal pain, odynophagia, penile oedema, and skin and anorectal abscesses. Most patients have a self-limited illness; between 1% and 13% require hospital admission (for treatment or isolation), and the case-fatality rate is less than 0·1%. A diagnosis can be made through the presence of Orthopoxvirus DNA in PCRs from lesion swabs or body fluids. Patients with severe manifestations and people at risk of severe disease (eg, immunosuppressed people) could benefit from antiviral treatment (eg, tecovirimat). The current strategy for post-exposure prophylaxis or pre-exposure prophylaxis for people at high risk is vaccination with the non-replicating modified vaccinia Ankara. Antiviral treatment and vaccines are not yet available in endemic countries in Africa.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}